Myth or Real? The Potential Serious Side Effects of Ticagrelor
Wassam EL Din Hadad EL Shafey
Wassam EL Din Hadad EL Shafey*
Cardiology Department, Menoufia University, Egypt
- *Corresponding Author:
- Wassam EL Din Hadad EL Shafey
Faculty of Medicine
Cardiology Department
Menoufia University
St Al Amin, Al Hayaa Pharmacy, Egypt
Tel: +201006420955
E-mail: dr_wesamhadad@yahoo.com
Abstract
Ticagrelor, a novel direct, reversibly binding P2Y12 antagonist, has better pharmacodynamic effects and improves clinical outcomes compared with clopidogrel in the setting of ACS. However, ticagrelor-related dyspnea and bradyarrhythmias have been observed in the PLATO trial, here in my case I will present a case of ticagrelor side effects and how it may burden the course of hospital stay.
Keywords
Ticagrelor, Side effects, ACS
Learning Objectives
Ticagrelor as a novel antiplatelet should be used in it is on label use only as it has some side effect that may add health and cost burden.
Introduction
Ticagrelor is a novel, potent, direct P2Y12 antagonist with rapid onset of action and intense, consistent platelet reactivity inhibition. In patients with ACS ticagrelor was superior to clopidogrel in decreasing major adverse cardiac events.[1] Therefore, ticagrelor (together with another P2Y12 inhibitor prasugrel) is preferred over clopidogrel [2] and is widely used in the setting of ACS.
In the landmark PLATO trial ticagrelor was linked to increased incidence of ventricular pauses which were predominantly asymptomatic.3 Here we report a case of ticagrelorassociated complete atrioventricular block in a patient with ACS which required resuscitation and insertion of temporary pacemaker and also atrial fibrillation.
Case Presentation
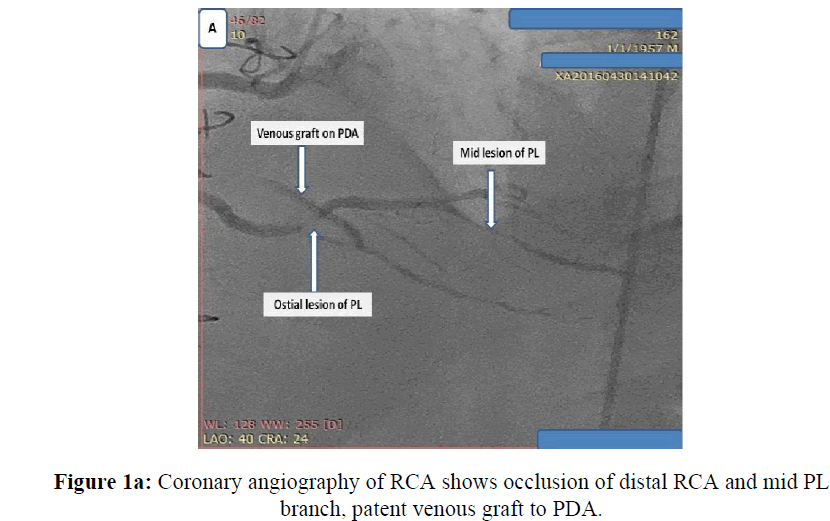
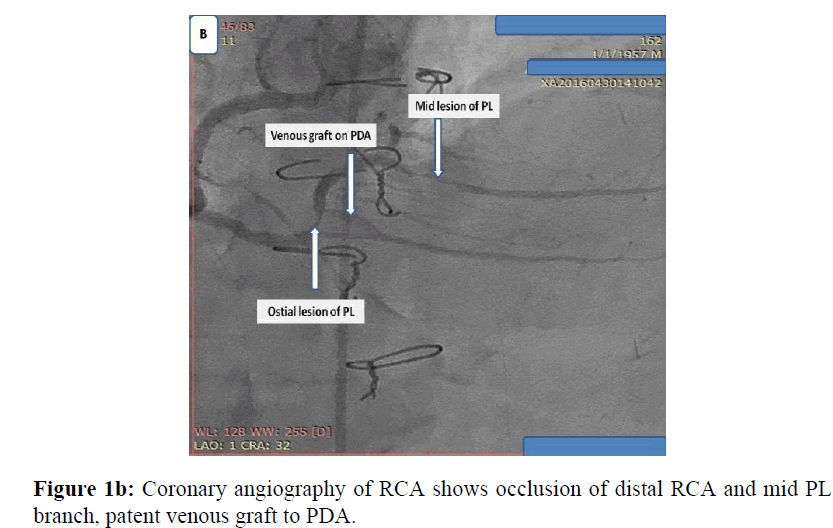
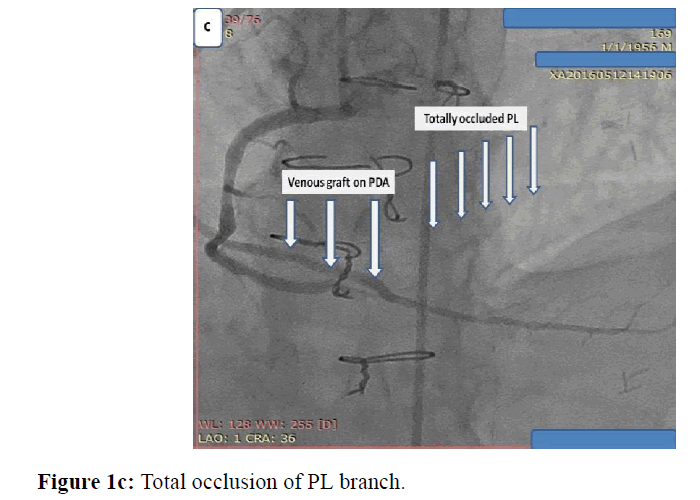
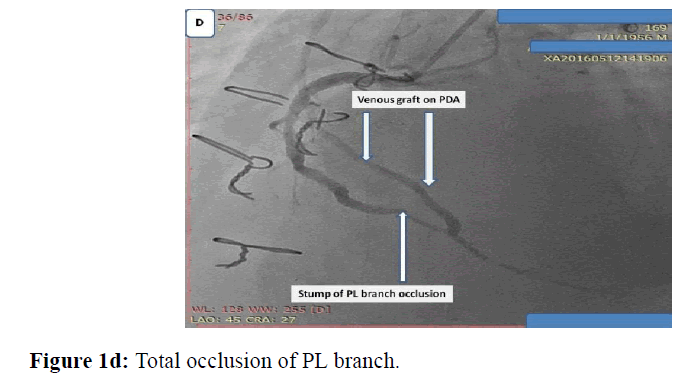
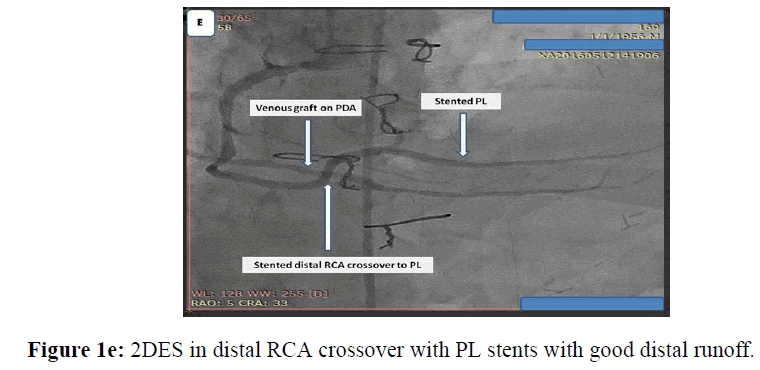
Male patient 59 years old, chronic heavy smoker, insulin dependent Diabetes mellitus, dyslipidemic, hypertensive and ischemic heart disease with previous CABG 5 years ago, presented with typical chest pain, positive cardiac markers and ST segment depression, coronary angiography was done and revealed total occlusion of native LAD, OM and distal RCA, patent LIMA graft and venous grafts to both OM and PDA. While RCA proper showed high thrombus burden all over its course, I decided to put the patient on GPIIb, IIIa infusion for 48 hours and redo control angiography, loading dose of ticagrelor 180 mg was given and maintained 90 mg twice daily, patient was kept with no symptoms till the 3rd day where he developed chest pain again, I decided to do re-angiography where I find distal occlusion of large PL branch which was patent before while RCA proper was cleared from thrombus, so I decided to do PCI to PL and distal RCA with 2 DES with good angiographic results (Figures 1a, 1b, 1c, 1d, 1e).
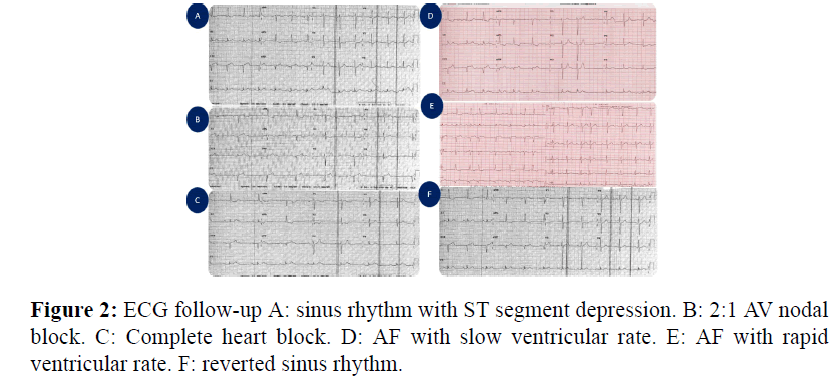
Chest pain was decreased dramatically after PCI, but in the first 24 h post PCI patient developed sinus bradycardia, he was on low dose bisoprolol 2.5 mg which was hold, then patient degenerated into different degrees of AV nodal block and finally into AF with controlled ventricular rate, along the time course of CCU stay (Figure 2).
Temporary pacemaker was inserted on demand mode and elective DC shocks to revert sinus rhythm were applied then IV loading and maintaining dose of amiodarone was given in a trial to maintain sinus rhythm. Before this dysrhythmia time course patient developed remarkable dyspnea of unexplained cause as bed side echocardiographic study showed good ventricular function and chest X-ray also where clear. Really it was the first time for me to use ticagrelor in daily practice and as if follow up cardiac markers were decreasing and chest pain totally vanished so I did not find any explanation except it may be the side effects of ticagrelor so, I started to switch the patient into clopidogrel and maintain follow up for more 2 days in the hospital, on the 3rd day before discharge sinus rhythm totally stabilized and dyspnea cleared totally and patient discharged home.
Discussion
Although the increased incidence of ventricular pauses associated with ticagrelor treatment has been previously reported, it is generally believed to be of no clinical importance.[3] Here I report a patient who developed severe symptomatic bradycardia with complete atrioventricular block after receiving a recommended loading dose of ticagrelor. The patient was unresponsive to medical treatment and required invasive temporary pacing. The atrioventricular block resolved completely after the discontinuation of the drug. My patient was on chronic beta-blocker therapy that could potentiate the influence of ticagrelor on cardiac conduction; although none of these is considered contraindication to ticagrelor therapy. Also, many patients with acute coronary syndrome receive beta blockers and conduction disturbances are not rare in this population. The mechanism of bradyarrhythmic effect of ticagrelor is poorly understood. [3] One possibility is a direct effect of ticagrelor on cardiac automaticity and conduction. The other one implicates an adenosine mediated effect. Ticagrelor inhibits cellular uptake and increases plasma concentration of adenosine,[4] which has a potent atrioventricular blocking effect. As such, adenosine is widely used as a diagnostic and therapeutic agent (e.g., in patients with supraventricular tachycardia).Therefore, increase in adenosine levels in patient treated with ticagrelor could be a plausible explanation for its effect on cardiac conduction.
My case demonstrates that bradyarrhythmic effects of ticagrelor can have important (although rare) clinical consequences. I would advise caution and careful observation of patients after initiating of ticagrelor therapy, especially in patients with already compromised conduction system or treated with medications with atrioventricular blocking properties.
Conflict of Interest
No
References
- Held C., Asenblad N., Bassand JP., Becker RC., Cannon CP., et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes undergoing coronary artery bypass surgery: results from the PLATO (Platelet Inhibition and Patient Outcomes) trial. J Am CollCardiol 2011; 57:672-684.
- Hamm CW., Bassand JP, Agewall S.,Bax J.,Boersma E., et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation. Eur Heart J 2011; 32: 2999–3054.
- Scirica BM., Cannon CP., Emanuelsson H., Michelson EL., Harrington Ra., et al. The incidence of bradyarrhythmias and clinical bradyarrhythmic events in patients with acute coronary syndromes treated with ticagrelor or clopidogrel in the PLATO (Platelet Inhibition and Patient Outcomes) trial: results of the continuous electrocardiogram. J AmCollCardiol 2011; 57: 1908–1916.
- Bonello L., Laine M., Kipson N., Mancini J., Helal O., et al.Ticagrelor increases adenosine plasma concentration in patients with an acute coronary syndrome. J Am CollCardiol 2014; 63: 872–877.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences