Uptake of pre cervical cancer screening service and associated factors among women aged 30-49 years in Finote Selam town northwest Ethiopia
Alehegn Bishaw Geremew, Abebaw Addis Gelagay, Telake Azale
Alehegn Bishaw Geremew1*, Abebaw Addis Gelagay1 and Telake Azale2
1Department of Reproductive Health, Institute of Public Health, College of Medicine and Health Science, University of Gondar, Ethiopia
2Department of Behavioral Science, Institute of Public Health, College of Medicine and Health Science, University of Gondar, Ethiopia
- *Corresponding Author:
- Alehegn Bishaw Geremew
Department of Reproductive Health, Institute of Public Health, College of Medicine and Health Science, University of Gondar, Ethiopia
E-mail: alexbishaw@gmail.com
Abstract
Background: Pre cervical cancer screening is one of cervical cancer prevention strategies. Screening service in Finote Selam general hospital has been started since April 2016, however, there is no evidence on cervical cancer screening uptake in the study area. Thus determining screening uptake is essential for programme effectiveness.
Objectives: The aim of this study was to assess uptake of pre cervical cancer screening and associated factors among women aged 30-49 year in Finote Selam northwest Ethiopia.
Methods: A community based cross-sectional study was conducted from March 30, 2017- April 15.2017 among 1152 participants. A cluster sampling technique was used to requite the desired sample size. The data were enter Epi-Info version 7 and exported to SPSS version 20 for analysis. Binary logistic regression model was fitted to identify factors associated with the uptake of pre cervical cancer screening. Odds ratio with 95 % confidence interval was used to identify strength and direction of association between outcome and covariates.
Results: In this study a total of 1137 out of 1152 women aged 30-49 years were participated representing a response rate of 98.7%. The uptake of pre cervical cancer screening was 34(3%) with 95% CI 2-4.2.
In the final model of analysis women had ≥ 5 pregnancy history was 80% (AOR=0.2, 95%CI: 0.004-0.7) less likely than who hand no any history of pregnancy to had uptake of screening service. Participant with history of sexually transmitted disease 12 (AOR=12, 95% CI: 4.3-24)times more likely to uptake screening service as compared with who and no history of sexually transmitted disease. Women who had awareness on pre cervical cancer screening was 16(AOR=16, 95% CI: 1.5-18) times more likely to uptake screening service as compared who had no awareness.
Conclusion and recommendation: Uptake of pre cervical cancer screening is low in the study area. Women had history of pregnancy ≥ 5 negatively associated with uptake of screening and history of sexually transmitted disease, awareness on screening service and favorable attitude towards screening positively associated with uptake of pre cervical cancer screening. Providing information to the women about cervical cancer screening and service availability near they lived is warranted.
https://bluecruiseturkey.co
https://bestbluecruises.com
https://marmarisboatcharter.com
https://bodrumboatcharter.com
https://fethiyeboatcharter.com
https://gocekboatcharter.com
https://ssplusyachting.com
Keywords
Women age 30-49 year’s; Pre cervical cancer; Uptake of screening
List of abbreviations
AOR: Adjusted Odds Ratio; CI: Confidence Interval; COR: Crude Odds Ratio; ETB: Ethiopian Birr; HIV: Human Immune Deficiency Virus; HPV: Human Papilloma Virus; SD: Standard Error; SPSS: Statistical Package of Social Science; VIA: Visual Inspection with Acetic Acid
Background
Cervical cancer is a public health problem, worldwide in 2013 an estimated to 236,000 death is reported more over 485,000 women were diagnosed with cervical cancer [1]. It is the second most common cancer in less developed region and remained the most common cancer in east and middle Africa [2]. Early onset of sexual intercourse, multiple sexual partner, human immunodeficiency virus (HIV) infection, history of sexual transmitted disease, human papiloma virus (HPV) infection, cigarette smoking and long term oral contraceptive use are considered risk factors for cervical cancer [3,4]. The age standardized rate of cervical cancer in sub-Saharan country is 30 per 100,000 women [5].
Variation in distribution of cervical cancer reflects differences in the accessibility of cervical cancer screening service and uptake of screening service [6]. Low socio economic status of the society also contribute high risk of the for the development of the disease [7]. The average proportion of cervical cancer screening in developing country is 19% compared to 63% in developed country and range from 1% to 73%.8 Screening ranged from 20% in urban to 2% in rural sub-Saharan country [5].
A Meta-analysis study found that the risk of dying from cervical cancer was 35% lower among women invited to screening with cytology testing than among women not offered screening [9]. In Ethiopian the outpatient and inpatient mean cost of cervical cancer treatment per person were $407.2 and $404.4 respectively [10].
Pre cervical cancer screening is one of the best prevention strategies of cervical cancer through early intervention of pre malignant lesion [11]. Screening service is recommended to be performed for sexually active female age 21-65 years at least once for every five year, if the three consecutive screening results are negative screening after women age greater than 65 years old is not necessary [12]. Human papilloma virus (HPV) Screening, cytology and visual inspection with acetic acid are the recommended screening test [13-15].
However, Currently in Ethiopia Cervical cancer screening test for women age 30-49 years and HIV positive women is recommended by Visual inspection with acetic acid (VIA) and pap smear followed by cryotherapy as methods of screening and treatment for precancerous lesions is preferred approach respectively [16]. The challenge for screening with VIA is failure to treat positive result with cryotherapy [17].
Women knowledge on cervical cancer disease, awareness, attitude towards pre cervical cancer screening and cost of screening service are the determinants for the uptake of pre cervical cancer screening service [18-20]. Heath education is potential intervention strategies to increase preservice cancer screening uptake among eligible women in the demand side [21].
National pre cervical cancer screening has been started in Ethiopia; Finote Selam general hospital has been started screening service provision in April 2016. However, evidence on pre cervical screening uptake yet not known in the study area. Therefore, community based study was employed to assess the uptake of pre cervical cancer screening and associated factors among women aged 30-49 years live in Finote Selam town, Northwest, Ethiopia.
Methods
Study design and period
A community based cross-sectional study was conducted from March 30, 2017- April 15, 2017.
Study setting
Study was conducted at Finote Selam town, Northwest, Ethiopia. Finote Selam town is located in west Gojam zone in Amhara regional state, Northwest, Ethiopia. The health facilities found in Finote Selam town are one primary Hospital, one public health centre and four private clinics. A pre-cervical cancer screening and treatment for pre cervical lesion with cryotherapy has been given at the hospital starting from April 2016.
The sources of population for the study were women aged 30-49 years live in Finote Selam town. Women age 30-49 years and who lived in Finote Selam town at least for 6 month was included for the study, whereas women age 30-49 years that were severely ill and unable to communicate effectively were excluded.
Sample size determination
The sample size was determined by using single population proportion formula with assuming that estimated proportion of pre cervical cancer screening uptake 8.3% from previous study in Ethiopia, 95% level of confidence, 2% of degree of precision, 5% none response rate, design effect of 1.5 [20].
n= (Zά/2)2 p(1-q)/d2
n=731
Where ά is level of significant
Z= Standard normal distribution curve value for 95% confidence level=1.96
p is proportion of pre cervical cancer screening uptake
d is degree of precision (0.02)=2 %
Therefore, the final required minimum sample size was estimated to be 1152 women aged 30-49 years. Sample size was also calculated for factors associated with pre cervical cancer screening by epi-info with the assumption of factors associated to cervical cancer from previous study in Dessie Ethiopia, power 80%, 95% CI and ration 1. However the calculated sample sizes for factors found to be less than sample size for proportion. Therefore by considering 1.5 design effect and 5% non-response rate, the final required minimum sample size was estimated to be 1152 women aged 30-49 years.
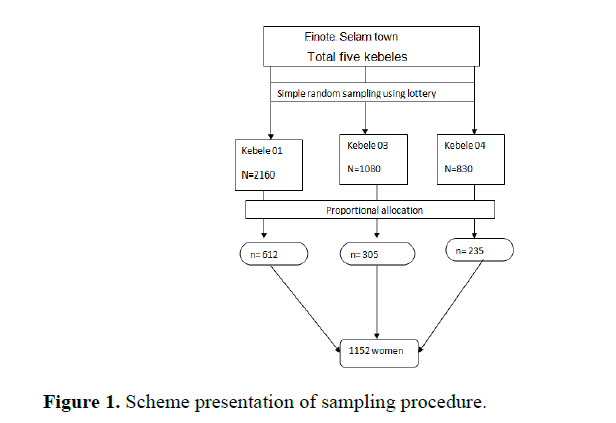
Sampling procedure
Three out of five clustered kebele selected by lottery method and proportionally allocated cluster sampling technique was employed to select the 1152 study participants from the three clusters (Figure 1).
Data collection instrument and process
The questionnaire was prepared in English by reviewing literatures and translated to Amharic language.
The content of questionnaire were socio-demographic characteristics, risk of exposure to cervical cancer and reproductive history, cervical cancer knowledge, screening awareness and attitude towards pre cervical cancer screening and uptake of screening practice questions. Six data collectors and two supervisors were involved in the data collection processes. Data were collected at home or near home shop using face to face interviewer administered questionnaire to considered illiteracy women.
Data quality control
The quality of data were ensured by translating the English version questionnaires to local language Amharic and providing a two day training for data collectors and supervisors on the technique of data collection and the approach to study participants. The questioners were pretested to check the response, language clarity and modification was done accordingly. Each process of data collection was checked by supervisors and the overall data collection process was checked by investigators on daily basis to ensured completes and consistency of the collected data.
Measurements
Woman considered uptake of pre cervical cancer screening if hand ever been screened for pre cervical cancer lesion in her life time.
Women knowledge on cervical cancer disease was determined by using different questions about risk factor, symptoms, prevention and treatment of cervical cancer disease. Women considered knowledgeable if they answered knowledge questions above the mean value. Women had ever heard on pre cervical cancer screening is considered have awareness on pre cervical cancer screening. Attitude towards pre cervical cancer screening was measured using different attitude questions and woman answered above the mean value was considered having favourable attitude towards pre cervical cancer screening (the detail is available in the previous published article) [22].
Data analysis process
The data were checked for completeness, coded manually and then entered to EPI-info version 7 and transferred to Statistical Package of Social Science (SPSS) version 20 for analysis. Descriptive statistics were expressed in numerical value, mean, Standard deviation, and percentage. Logistic regression analysis was done to identify variables associated with cervical precancerous screening uptake. Statistically associated variable at p-value <0.05 from bivariate analysis was entered in multivariable analysis to control potential confounders. Multivariable model was tested for goodness of fit with Hosmer- Lemeshow test. Adjusted odds ratio with 95% confidence interval was used to determine the degree and direction of association between covariates and pre cervical screening up take.
Results
Socio demographic characteristics of the participants
A total of 1137 out of 1152 women participated in the study with 98.7% response rate. Their mean age was 37.4 years (SD=5.72 years). Majority (65%) of participants age was 30-39 year and almost all (92.2%) of the study participants were orthodox by religion, one-third (33.6%) of the women were single. Approximately half of participants (45.1%) of them had no formal education while 329(28.9%) had secondary school and above. Out of the total participants 425(37.4%) of them occupational status was employed (self, private and government employed). More than half (58.2%) of study participants average family monthly income was less than 1500 Ethiopian birr (Table 1). Out of women aged 30-39 years 3.4 % had pre cervical cancer screening uptake and 2.3% among women aged 40-49 years. Screening up take by marital status: 3.1% single and 2.9% married women had pre cervical cancer screening uptake. Screening status by education: 1.2% women with no formal education, 3.7% women had primary education and 5.2% women had secondary and above education had screened for pre cervical cancer. A proportion of 8.2% employed and 1.4% of unemployed women had also screened for pre cervical cancer (Table 1).
| Characteristics | Frequency n=1137 (%) | Screening uptake | P-value | |
|---|---|---|---|---|
| Yes | No | |||
| Age | ||||
| 30-39 | 738 (64.9) | 25 (3.4) | 713 (96.6) | 0.28 |
| 40-49 | 399 (35.1) | 9 (2.3) | 390 (97.7) | |
| Religion | ||||
| Orthodox | 1048 (92.2) | 27 (2.6) | 1021 (97.4) | |
| Others | 89 (7.8) | 7 (7.8) | 82 (92.2) | 0.008 |
| Marital status | ||||
| Single | 382 (33.6) | 12 (3.1) | 370 (96.9) | |
| Married | 755 (66.4) | 22 (2.9) | 733 (97.1) | 0.8 |
| Educational status | ||||
| No formal education | 513 (45.1) | 6 (1.2) | 507 (98.8) | |
| Primary school | 295 (26) | 11 (3.7) | 284 (96.3) | 0.021 |
| Secondary school and above | 329 (28.9) | 17 (5.2) | 312 (94.8) | 0.001 |
| Occupation | ||||
| Unemployed | 543 (47.8) | 8 (1.4) | 535 (98.6) | |
| Self employed | 423 (37.2) | 12 (2.8) | 411 (97.2) | 0.14 |
| Employed | 171 (15) | 14 (8.2) | 157 (91.8) | 0 |
| Family average monthly income* | ||||
| <1500 | 662 (58.2) | 19 (2.5) | 714 (97.5) | |
| = 1500 | 475 (41.8) | 15 (3.7) | 389 (96.3) | 0.29 |
| *ETB, Others: Muslim, protestant and catholic | ||||
Table 1: Socio-demographic characteristics of women aged 30-39 years live in Finote Selam town, northwest Ethiopia, 2017.
Women risk of exposure to cervical cancer and reproductive history
The mean age of first sexual intercourse of the women was 16.4 years ± (SD 3.29 years). Out of the participants more than half of the women 615 (54.1%) had the first sexual intercourse at the age of sixteen or below. Women sexual history, 788 (69.3%) had two or more sexual partner in their life time. Only 49 (4.3%) of women self-reported history of sexually transmitted disease. Out of the participants 166 (14.6%) of women had history of oral contraceptive use. Among the total participants 1016 (89.4%) women had at least one history of pregnancy and (88%) women had history of at least one child birth, and 20% of women had grand multiparty.
Knowledge of cervical cancer and attitude towards pre cervical cancer screening
Out of the participants 30.3% had knowledge on cervical cancer and the proportion of women who had favorable attitude towards cervical cancer screening was 58.1 %( The detail is available on previously published article) [22].
Awareness on pre cervical cancer screening and pre cervical cancer lesion treatment
Women’s awareness about pre cervical cancer screening was only 278 (24.5%) (95% CI: 21.9, 27). The dominant source of information for screening was health provider 108 (38.8%), followed by family friends, neighbors 95 (34%), mass media (29.8%) and printed material (4%) are also the source of information.
Among participants who heard pre cervical cancer screening, 128 of them identified that sexually active women aged 30 year and above are eligible for pre cervical cancer screening, 30 identified that HIV positive women are eligible to be screened. 8 of them also identified that prostitute women are eligible for screening, but 104 of the participant did not now any eligibility for pre cervical cancer screening.
Regarding time interval of screening among women ever heard cervical cancer screening 68 (24.5%) of correctly mentioned screening interval. Out of pre cervical cancer screening ever heard women 52 (18.7%) were identified at least one screening methods. The types of screening methods mentioned by participants were visual inspection with acetic acid (VIA) and Pap smear. The visual inspection with acetic acid was frequently mentioned screening method (73%). Two-third (67.6%) of women though that being positive for pre cervical cancer screening is indicated women has cervical cancer.
Uptake of pre cervical cancer screening service
The number of women who had ever examined for any gynecological problem like vaginal bleeding and STI in their life time was 217 (19.1%). Among those examined for gynecological problem majority of participants 169 (77.8%) was visited hospital for examination.
Among women participated in the study only 34 (3%) (95% CI: 2, 4.2) of women were screened for pre cervical cancer lesion in their life time. Regarding frequency of screening among screened women 31 (91% were screened a single time and 9% were screened two times. Out of women who were screened for Pre cervical cancer 23 (67.6%) were initiated to be screened by health provider and 9 (26.4%) of them selfinitiated and the others motivated by friends 5.8%. The 88% of women were screened in hospital where as 12% were screened in private clinic.
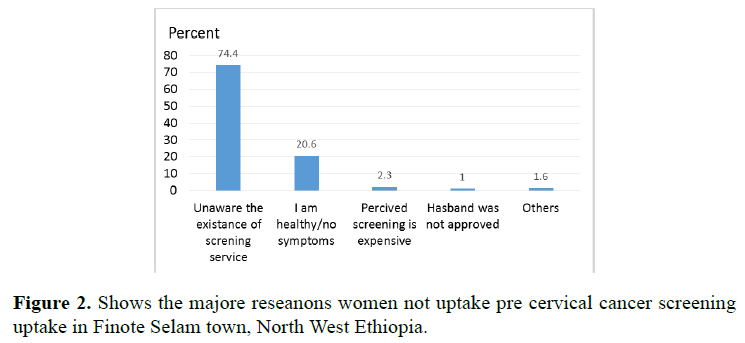
The frequent reason women mentioned not being screened for cervical cancer was unawareness on the existence of the screening service 821 (74.4%), followed by perceived healthy/absence of early cervical cancer symptom 228 (20.7%) (Figure 2).
Factors associated with uptake of pre cervical cancer screening service
From bivariate analysis variables such as: educational status, occupational status, knowing any one with cervical cancer, pregnancy history, gravidity, ever used modern contraceptive, history of sexually transmitted disease, knowledge on cervical cancer, awareness on pre cervical cancer screening and attitude toward pre cervical cancer screening were statistically and significantly associated with pre cervical cancer screening service uptake of the participants. In multivariable analysis remained independently associated with pre cervical cancer screening service uptake.
Women who had history of pregnancy ≥ 5 was 80%(AOR=0.2, 95% CI: 0.04-0.7) less likely to cervical cancer service up take as compared to women who hand no any pregnancy history. Study participants with history of sexually transmitted disease 12(AOR=12, 95% CI: 4.3-24) times more likely to have pre cervical cancer screening service uptake compared to had no history of sexually transmitted disease. Awareness on pre cervical cancer, women who had ever heard about pre cervical cancer was 9 (AOR=9, 95% CI: 1.5-18)times more likely to had pre cervical cancer screening service uptake as compared to who had never heard about the screening service. Having favourable attitude towards pre cervical cancer screening is 9(AOR=9, 95% CI: 1.5-18) times more likely to uptake pre cervical cancer compared with its counterpart (Table 2)
| Factors | Screening uptake | COR | 95% CI | AOR | 95% CI | |
|---|---|---|---|---|---|---|
| No | Yes | |||||
| Educational status | ||||||
| No formal education | 507 | 6 | 1 | 1 | ||
| Primary school | 284 | 11 | 3.2 | 1.19-8.94 | 1.1 | 0.2-4.2 |
| Secondary and above | 312 | 17 | 4.6 | 1.8-11.8 | 1.3 | 0.6-1.5 |
| Occupational status | ||||||
| Unemployed | 535 | 8 | 1 | 1 | ||
| Self employed | 411 | 11 | 1.9 | 0.79-4.8 | 1.3 | 0.4-4.5 |
| Gov/private Employed | 157 | 14 | 6 | 2.5-14.4 | 3.7 | 0.8-17 |
| Knowing any one with CCa | ||||||
| No | 1048 | 25 | 1 | 1 | ||
| Yes | 55 | 9 | 6.8 | 3.05-15.4 | 1.04 | 0.3-3.5 |
| Pregnancy history | ||||||
| No | 106 | 15 | 1 | 1 | ||
| Yes | 997 | 19 | 0.13 | 0.06-0.27 | 1.3 | 0.4-7.5 |
| Gravidity | ||||||
| 0 | 106 | 15 | 1 | 1 | ||
| 1 | 121 | 13 | 0.17 | 0.49-.62 | 0.26 | 0.08-1.9 |
| 4-Feb | 649 | 11 | 0.12 | 0.05-0.27 | 0.23 | 0.03-1.5 |
| = 5 | 227 | 3 | 0.15 | 0.05-.44 | 0.2 | 0.04-0.7* |
| Ever use modern contraceptive | ||||||
| No | 304 | 3 | 1 | |||
| Yes | 799 | 31 | 3.9 | 1.19-12.9 | 1.03 | 0.2-4.5 |
| History of STD | ||||||
| No | 1072 | 16 | 1 | 1 | ||
| Yes | 31 | 18 | 38 | 18-83 | 12 | 4.3-24.00** |
| Knowledge on cervical cancer | ||||||
| Not knowledgeable | 790 | 2 | 1 | 1 | ||
| Knowledgeable | 313 | 32 | 40 | 39.6-169 | 3.7 | 0.4-27 |
| Ever heard pre cervical cancer screening | ||||||
| No | 857 | 2 | 1 | 1 | ||
| Yes | 246 | 32 | 55 | 13-234 | 16 | 2.4-18* |
| Attitude towards pre cervical cancer screening | ||||||
| Not favourable | 475 | 1 | 1 | 1 | ||
| Favourable | 628 | 33 | 24.9 | 3.4-183 | 9 | 1.5-18* |
| CCa: Cervical Cancer; COR; Crude Odds Ratio; CI: Confidence Interval; AOR: Adjusted Odds Ratio;1: Reference category; STD: Sexually Transmitted Disease **: 0.001<p<0.05; **: p<0.001 |
||||||
Table 2: Bivariate and multivariable analysis of factor associated with cervical cancer screening uptake among women aged 30-49 years Finote Selam town, northwest Ethiopia, 2017.
Discussion
Pre cervical cancer screening has great role in reduction of cervical cancer disease and death due to the disease, however, cervical cancer screening uptake is low in Finote Selam town. The screening uptake varies across the countries, in average 19% developing country to 63% in developed country [8]. Thus this study aimed to identify pre cervical cancer screening uptake and associated factors among women aged 30-49 years.
Study participants had ever heard about cervical cancer screening in our study was only 24.5% which is in line with finding reported from Zimbabwe [23], and Gabon [24], but much lower than finding reported from Kenya [25]. The possible explanation the observed difference could be due to national cervical cancer screening program initiated recent time in Ethiopia including the study area.
In our study only 3 %( 95% CI: 2-4.2) of women were uptake pre cervical cancer screening service in their life time. Which is consistent with studies in Nigeria [26], Laos PDR [27], however, better than study conducted in Ghana among female age 10-74 years [28], but lower than a study finding conducted in developing countries8,(Nepal [29], India [30], this gap from other countries studies might be national cervical cancer screening program initiated recent time and less advocacy activities were done in Ethiopia. Our study also lower than study conducted in Dessie Ethiopia [20], Mekele [31] Addis Ababa [32]. The possible explanation for the difference study done in Dessie might be due to study participants were hospitalized client might be more on screening service and study conducted in Mekele could be due to it was Addis Tesfa project area for platform action [33], while study in Addis Ababa the participants were women with HIV visit health facility. From multivariable logistic regression analysis women history of pregnancy, gravidity ≥ 5 was 80% less likely to uptake pre cervical cancer screening as compared to who hand no any history pregnancy. This might due to perception of multi gravida women cervical cancer screening is concerned for null gravida and infertile women.
Study participants with history of sexually transmitted disease 12(AOR=12, 95% CI: 4.3-24) times more likely to have pre cervical cancer screening service uptake compared to had no history of sexually transmitted disease. This finding is supported by other studies [31,34,35].
Awareness on pre cervical cancer screening, women who had ever heard about pre cervical cancer screening was 16 (AOR=16, 95% CI:2.4-18) times more likely to had pre cervical cancer screening service uptake as compared to who had never heard about the screening service. Consistent finding reported from other studies [36-38]. Having favorable attitude towards pre cervical cancer screening is 9(AOR=9, 95% CI: 1.5-18) times more likely to uptake pre cervical cancer compared with its counterpart. This is finding is supported by evidences [19,39,40].
Conclusion and Recommendation
Cervical cancer is a measure public health problem, however, in this study we identified that women uptake of pre cervical cancer screening is found to be low in Finote Selam town, the frequent reason women mentioned not to screen for cervical cancer were unawareness of screening service and perceived healthy. Women had history of pregnancy ≥5 negatively associated with uptake of screening and history of sexually transmitted disease, awareness on screening service and favorable attitude towards screening positively associated with uptake of pre cervical cancer screening.
Providing information to the women about cervical cancer screening and service availability near they lived by using mass media, leaflet and including screening service availability during health education program.
Declaration
Ethical approval and consent to participate
Ethical clearance was obtained from Institutional Review Board University of Gondar, Institute of public health. Verbal informed consent was secured from every study participant before data collection and participation was on voluntary basis and they can refuse or withdraw from the study at any time if they were not comfortable to participant in the study. Confidentiality of any information provided by study participants was maintained throughout the study by excluding personal identifiers from the data collection form and making collected data inaccessible except data collectors, supervisors and authors.
Consent for Publication
It is not applicable.
Availability of Data and Material
All the required data are available in the main document.
Competing Interest
Authors declared that have no any competing interest including financial interest.
Funding
The study budget was secured from university of Gondar.
Author Contributions
ABG develop the proposal, conduct the data analysis and ABG, AAG, and TA equally contributed during drafting and revising the manuscript and finally all the authors read and approved for their work.
Acknowledgements
We would like to extend our heart full gratitude to University of Gondar, Institute of public health for giving ethical clearance to us. Our heart full tanks extended to study participants for their time and willingness to participate and to data collectors and supervisor for their commitment to work. Our appreciation also for Finote selam town health office their willingness for ours data collection.
References
- Fitzmaurice C, Dicker D, Pain A, Hamavid H, Moradi-Lakeh M, MacIntyre MF, et al. The Global Burden of Cancer 2013. JAMA Oncol. 2015; 1: 505-527.
- Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. International journal of cancer. 2015; 136: E359-E386.
- DeCherney A, Nathan L, Goodwin TM, Laufer N: Current diagnosis and treatment obstetrics and gynecology: McGraw-Hill Medical. 2012.
- Getinet M, Gelaw B, Sisay A, Mahmoud EA, Assefa A. Prevalence and predictors of Pap smear cervical epithelial cell abnormality among HIV-positive and negative women attending gynecological examination in cervical cancer screening center at Debre Markos referral hospital, East Gojjam, Northwest Ethiopia. BMC Clin Pathol. 2015; 15:16.
- Louie KS, De Sanjose S, Mayaud P. Epidemiology and prevention of human papillomavirus and cervical cancer in sub-Saharan Africa: a comprehensive review. Tropical Medicine & International Health. 2009;14: 1287-1302.
- Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA: a cancer journal for clinicians. 2015; 65: 87-108.
- McGuire S. World Cancer Report 2014. Geneva, Switzerland: World Health Organization, International Agency for Research on Cancer, WHO Press, 2015. Adv Nutr. 2016;7:418-419.
- Gakidou E, Nordhagen S, Obermeyer Z. Coverage of cervical cancer screening in 57 countries: low average levels and large inequalities. PLoS Med. 2008;5:e132.
- Peirson L, Fitzpatrick LD, Ciliska D, Warren R. Screening for cervical cancer: a systematic review and meta-analysis. Syst Rev. 2013;2:35.
- Hailu A, Mariam DH. Patient side cost and its predictors for cervical cancer in Ethiopia: a cross sectional hospital based study. BMC cancer. 2013;13:69.
- Jin XW, Lipold L, McKenzie M, Sikon A. Cervical cancer screening. Cleveland Clinic journal of medicine. 2013; 80:153-160.
- Smith RA, Andrews KS, Brooks D, Fedewa SA, Manassaram-Baptiste D, Saslow D. Cancer screening in the United States, 2018: A review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin 2018.
- WHO guidelines for screening and treatment of precancerous lesions for cervical cancer prevention. 2014.
- WHO: Comprehensive Cervical Cancer Control A guide to essential practice. Second edition. 2014.
- Organization WH: WHO guidelines for screening and treatment of precancerous lesions for cervical cancer prevention: supplemental material: GRADE evidence-to-recommendation tables and evidence profiles for each recommendation. 2013.
- Federal Ministry of Health Ethiopia national cervical cancer prevention training package Participant manual.
- Msyamboza KP, Phiri T, Sichali W, Kwenda W, Kachale F. Cervical cancer screening uptake and challenges in Malawi from 2011 to 2015: retrospective cohort study. BMC Public Health 2016; 16: 806.
- Ndikom CM, Ofi BA. Awareness, perception and factors affecting utilization of cervical cancer screening services among women in Ibadan, Nigeria: a qualitative study. Reprod Health. 2012; 9:11.
- Ali RC, Mulumba P, Verdonck K, Vanden Broeck D, Praet M. Knowledge, attitude and practice about cancer of the uterine cervix among women living in Kinshasa, the Democratic Republic of Congo. BMC Womens Health. 2014;14:30.
- Andargie A, Reddy PS. Knowledge, Attitude, Practice and Associated Factors of Cervical Cancer Screening Among Women in Dessie Referral Hospital and Dessie Health Center, Northeast Ethiopia. Global Journal For Research Analysis. 2016; 4.
- Gan DE, Dahlui M. Cervical screening uptake and its predictors among rural women in Malaysia. Singapore Med J.2013; 54:163-168.
- Geremew AB, Gelagay AA, Azale T. Comprehensive knowledge on cervical cancer, attitude towards its screening and associated factors among women aged 30-49 years in Finote Selam town, northwest Ethiopia. Reproductive health. 2018; 15: 29.
- Mupepi SC, Sampselle CM, Johnson TR. Knowledge, attitudes, and demographic factors influencing cervical cancer screening behavior of Zimbabwean women. J Womens Health (Larchmt). 2011; 20: 943-952.
- Assoumou SZ, Mabika BM, Mbiguino AN, Mouallif M, Khattabi A, Ennaji MM. Awareness and knowledge regarding of cervical cancer, Pap smear screening and human papillomavirus infection in Gabonese women. BMC women's health. 2015; 15: 37.
- Nthiga AM: Determinants of cervical cancer screening uptake among women in Embu county, Kenya. 2014.
- Nwankwo K, Aniebue U, Aguwa E, Anarado A, Agunwah E. Knowledge attitudes and practices of cervical cancer screening among urban and rural Nigerian women: a call for education and mass screening. European journal of cancer care. 2011; 20: 362-367.
- Sichanh C, Fabrice Q, Chanthavilay P, Diendere J, Latthaphasavang V, Longuet C, et al. Knowledge, awareness and attitudes about cervical cancer among women attending or not an HIV treatment center in Lao PDR. BMC cancer.2014; 14:161.
- Ebu NI, Mupepi SC, Siakwa MP, Sampselle CM. Knowledge, practice, and barriers toward cervical cancer screening in Elmina, Southern Ghana. Int J Womens Health 2015; 7:31-39.
- Ranabhat S, Tiwari M, Dhungana G, Shrestha R. Association of knowledge, attitude and demographic variables with cervical Pap smear practice in Nepal. Asian Pac J Cancer Prev. 2014; 15: 8905-8910.
- Bansal AB, Pakhare AP, Kapoor N, Mehrotra R, Kokane AM. Knowledge, attitude, and practices related to cervical cancer among adult women: A hospital-based cross-sectional study. Journal of Natural Science, Biology and Medicine. 2015; 6: 324.
- Bayu H, Berhe Y, Mulat A, Alemu A. Cervical Cancer Screening Service Uptake and Associated Factors among Age Eligible Women in Mekelle Zone, Northern Ethiopia, 2015: A Community Based Study Using Health Belief Model. PLoS One. 2016; 11: e0149908.
- Belete N, Tsige Y, Mellie H. Willingness and acceptability of cervical cancer screening among women living with HIV/AIDS in Addis Ababa, Ethiopia: a cross sectional study. Gynecol Oncol Res Pract. 2015; 2:6.
- Pathfinder international Combating Cervical Cancer in Ethiopia ,Addis Tesfa project. 2010.
- Aguilar-Perez JA, Leyva-Lopez AG, Angulo-Najera D, Salinas A, Lazcano-Ponce EC. Cervical cancer screening: knowledge of Pap smear benefits and utilization in Mexico. Rev Saude Publica. 2003; 37:100-106.
- Augusto EF, Rosa ML, Cavalcanti SM, Oliveira LH. Barriers to cervical cancer screening in women attending the Family Medical Program in Niteroi, Rio de Janeiro. Arch Gynecol Obstet. 2013; 287: 53-58.
- Chaowawanit W, Tangjitgamol S, Kantathavorn N, Phoolcharoen N, Kittisiam T, Khunnarong J, et al. Knowledge, Attitudes and Behavior of Bangkok Metropolitan Women Regarding Cervical Cancer Screening. Asian Pac J Cancer Prev. 2016; 17: 945-952.
- Compaore S, Ouedraogo CM, Koanda S, Haynatzki G, Chamberlain RM, Soliman AS. Barriers to Cervical Cancer Screening in Burkina Faso: Needs for Patient and Professional Education. J Cancer Educ. 2016; 31: 760-766.
- Mokhele I, Evans D, Schnippel K, Swarts A, Smith JS, Firnhaber C. Awareness, perceived risk and practices related to cervical cancer and Pap smear screening: A cross-sectional study among HIV-positive women attending an urban HIV clinic in Johannesburg, South Africa. S Afr Med J. 2016; 106: 1247-1253.
- Mukama T, Ndejjo R, Musabyimana A, Halage AA, Musoke D. Women’s knowledge and attitudes towards cervical cancer prevention: a cross sectional study in Eastern Uganda. BMC Women's Health. 2017; 17: 9.
- Basu P, Hassan S, Fileeshia F, Mohamed S, Nahoodha A, Shiuna A, et al. Knowledge, attitude and practices of women in maldives related to the risk factors, prevention and early detection of cervical cancer. Asian Pac J Cancer Prev 2014; 15: 6691-6695.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences