Seasonal Variations of Admission and Survival Status of Children Treated for Severe Acute Malnutrition (SAM) at Outpatient Therapeutic Program (OTP) in Wolaita Zone, Southern Ethiopia
Mulugeta Yohannis Kabalo, Misrak Mesfin Shanka
1School of Public Health, Wolaita Sodo University, Southern Ethiopia, P.O.Box 126, Wolaita Sodo, Ethiopia
2College of Public Health and Medical Sciences, Jimma University, Oromia Regional State, Ethiopia
- *Corresponding Author:
- Mulugeta Yohannis Kabalo
School of Public Health
Wolaita Sodo University, Southern Ethiopia
P.O.Box 126, Wolaita Sodo, Ethiopia
E-mail: yohannismulugeta@yahoo.com
Abstract
Background: Approximately 13 (2%) million children within developing countries suffer from severe acute malnutrition (SAM). The existing protocol brought SAM management from facility based approach to community based by means of Outpatient Therapeutic Program (OTP). But, little was known about seasonal variations of SAM admission in the program and survival status of children at OTP. Thus, this study aimed to investigate seasonal variations of SAM admission and survival status of children admitted to OTP in Wolaita Zone, Southern Ethiopia, 2015.
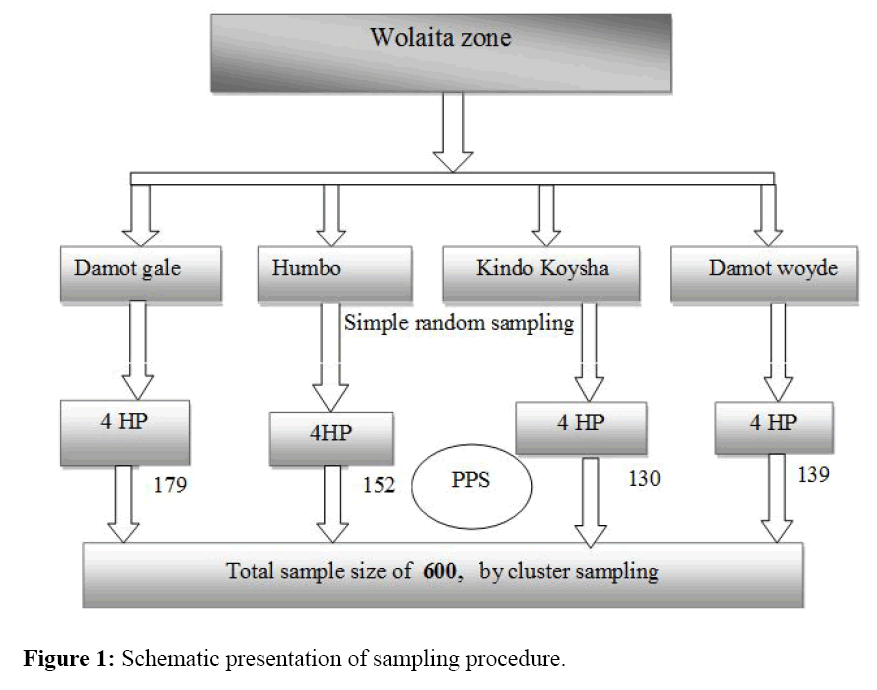
Methods: A retrospective facility based cross-sectional study was conducted in records of OTP in 2015. Six hundred (600) children represented by their OTP card were included from 16 health posts. Individual children card was selected by cluster sampling. Population Proportion to Size (PPS) allocation was used to assign sample for each selected Woredas and OTP sites in each Woreda. Data were entered, cleaned and analyzed in SPSS version 20.
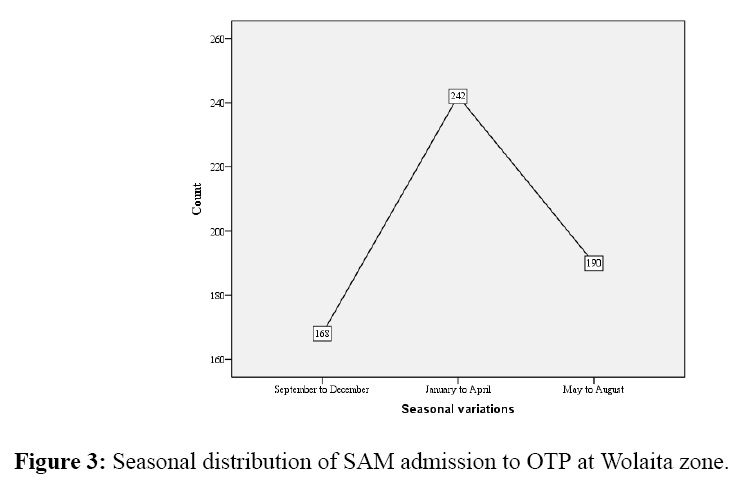
Results: Seasonal distribution of SAM admission to OTP in Wolaita Zone shows large quantities 242(40.3%) at 95% CI of (36.2, 44.2) admitted in January to April (summer season) of the year. The admissions at September to December (winter season) were 168(28.0%) at 95% CI of (27.8, 35.5) notified as least admission season. At the program, 396(66.0%) at 95% CI of (62.2, 69.8) children survived after complete length of stay. Children survival rate through time was affected in statistically significant figure by type of malnutrition and provision of supportive medications like amoxicillin at 95% confidence level in Log Rank test (P<0.05).
Conclusions: Based on the findings, large extents of children were admitted to the program in summer season of the year in the study area. The survival rate was lower compared to acceptable range of sphere standard. Besides, variables which affect the survival status of children were type of malnutrition and provision of amoxicillin. Therefore, stakeholders of the program should give attention for vulnerable seasons and intervention measures should be taken on factors affecting survival rate.
Keywords
Outpatient therapeutic program, Seasonal variations, Severe acute malnutrition, Survival status
Abbreviations
CMAM: Community based Management of Acute Malnutrition; EDHS: Ethiopian Demographic and Health Survey; MAM: Moderate Acute Malnutrition; MUAC Mid Upper Arm Circumference; NORHAD: Norwegian Agencies for Development; OTP: Outpatient Therapeutic Program; RUTF: Ready Used Therapeutic Food; SAM: Severe Acute Malnutrition; SNNPR: Southern Nation Nationalities People Region; TFC: Therapeutic Feeding Center; TSFP: Targeted Supplementary Feeding Program; UNICEF: United Nations Children Fund
Introduction
Malnutrition is defined as disorder resulting from a deficiency or excess of one or more essential nutrient [1,2]. In developing world this is usually described as under-nutrition whereby there exist varying degree of deficiencies in essential nutrients [3]. The body of children respond to under- nutrition by stunting, wasting and/or nutritional edema [4]. Acute malnutrition is the short term or acute response to inadequate nutritional intakes often occurs in combination with infections [3]. It is classified as moderate acute malnutrition(MAM) and SAM based on their severity [3]. The severity is designated by children Weight for Height Z-score, Weight for Height, presence of edema and Mid Upper Arm Circumference (MUAC). Acute malnutrition is called SAM when, Weight for Height Z-score <-3 or <70% median percentage, MUAC<11.5 cm or nutritional edema +/++/+++[5].
The prevalence of acute malnutrition in Oceania, Latin America, Asia and Africa were currently reported as 5%, 3%, 10% and 8% respectively [6]. Approximately 13(2%), million children living in developing countries mainly within Sub-Saharan group suffer from SAM [7]. According to Ethiopian Demographic and Health Survey (EDHS) report 2011, 10% under-five children were wasted and 3% severely wasted. The same report of EDHS in Southern Nations Nationalities and People Region (SNNPR) indicates the burden of wasting in under-five as 7.6% and children with severe wasting were 1.9% in SNNPR [8].
Acute malnutrition which includes both wasted and edematous cases were prevalent in study area, though the rates vary in specific Woredas. The burden of acute malnutrition was reported as 3.0% and 4.3% in Humbo and Sodo Zuria Woreda in 2007 [9]. Under-five children of Offa Woreda in 2004 were with acute malnutrition for 13.4% and SAM was reported as 0.4% [10]. Acute malnutrition in under-five children within Boloso Sore Woreda was 7.7% and particularly SAM was 1.4% in 2008 [11]. In Kindo Koysha and Boloso Bombe Woredas 12.4%, 10% and 3.2%, 2.2% acute malnutrition and SAM prevalence were reported respectively in 2008 [12]. SAM in children carries 9 times higher risk of death than a healthy child [3,4]. As indicated above it is public health problem in Wolaita Zone, Southern Ethiopia. It was previously managed in health facilities and therapeutic feeding centers(TFC) with its own difficulties [13,14]. The drawbacks in the previous management approach were expressed with its limited coverage, impact and costly to caregivers [7,15]. To reduce this limitations with previous management system, Community based Management of Acute Malnutrition (CMAM) was endorsed. Community outreach, outpatient care for the management of SAM without medical complications (OTP), inpatient care for the management of SAM with medical complications (SC) and the programme addresses MAM (Targeted Supplementary Feeding Program (TSFP)) were components of CMAM [5,7,14].
CMAM was endorsed in 2007 upon joint statements of World Health Organization (WHO) and United Nation Children Fund (UNICEF) [5,7,14]. The approach located management of SAM without complications and with appetite in OTP. This program serve SAM children aged 6–59 months with Ready Used Therapeutic Foods (RUTF) based on their weight and with other routine supportive medications [5,16]. Children fail appetite test and with medical complications are managed in inpatient bases until recovered from complications and return of appetite within stabilization center (SC)[7,17].
The effectiveness of SAM management was compared with international sphere standard cut off points [18]. Acceptable ranges of primary performance indicators of standard were >75%, <10% and <15%, recovery, death and default rates respectively [18]. The study in India reported, recovery rate 57.4%, death rate 0.8%, and default rate 36.2% in OTP [19]. Another similar large study done in Sub-Saharan Africa in OTP indicated, recovery, death and default rates of 74.2, 7.3 and 9.2% respectively [4]. The recovery rate 87% and death rate 3.6% were reports from study done within TFCs in SNNPR, in Ethiopia [13]. Likewise, recovery 61.78%, defaulter 13.85%, and death rates 3.02% from research done at OTP in Tigray region [16].
The management of SAM were influenced by many factors and varied with studies, areas and settings [20]. Treatment centers, type of malnutrition, co-morbidities and supportive medications provision were some of factors predicted as affecting treatment outcomes of SAM [13,16,21]. The study conducted in Tigray region reported as appetite test was associated with recovery rate from SAM. Children passed appetite test with RUTF were 4.5 times highly recovered at 95% CI(1.02, 19.62) when compared to children failed appetite test [16].
The performance of OTP for the management of SAM in children was hardly explored and factor associated with the performance of the program were also not significantly investigated in Ethiopia [16,22]. Since, the endorsement of the program there were little studies conducted to elucidate the effectiveness of OTP in the country. But as indicated, SAM was identified as public health problem in SNNPR particularly in Wolaita Zone and the program implementation was also since piloting time. Additional to lack of program effectiveness findings in large, seasonality of the problem was assessed hardly in this region of the country. However, the information need of program performance and variation of the problem load through time for stakeholders were straightforward. Therefore, the level of treatment outcome, survival status of children through time and seasonal variations of SAM admission in OTP oblige to be studied in Southern Ethiopia.
Currently, there is very little descriptive information available in current treatment outcome level of children managed from SAM at OTP in Ethiopia. But, seasonal variation of SAM admission to OTP was not investigated yet. Therefore, this study fills the information gaps through exploring seasonal variation of admission to OTP and survival status at OTP through time. That would add significant input for the program and policy makers to set long term planning for CMAM services in general and OTP in particular. Hence, this study was done to explore seasonal variations of SAM admission and survival status of children admitted to the program in Wolaita Zone, Southern Ethiopia, 2015.
Methods and Materials
Study area
The study was conducted in Wolaita Zone, Southern Ethiopia. The study area is one of zonal administrations in Southern region of the country, located in 390 kms south of Addis Ababa. Total population of this study area was estimated for about 2 million, where 52% were females and about three hundred thousands were children under-five years of age. The annual report of zonal health department indicates nearly about 20,000 under five SAM children were managed at OTP in 2015. The study area in general has 12 managerial Woredas and 3 town administrations. Likewise this area share five Hospitals, 75 Health Centers, and about 390 Health Posts [23].
Study design and period
Retrospective crossectional study was conducted on records from January to December in 2015, at Wolaita administrative Zone.
Source and study population
All children admitted to OTP of Wolaita Zone, with a diagnosis of SAM in 2015 were source population. All selected SAM children from specific selected OTP sites were study populations.
Inclusion and exclusion criteria
SAM children admitted to OTP from January to December 2015 were included. Children who were readmitted were excluded from the study.
Sample size determination and sampling procedure
Sample size for this study was calculated based on assumptions of single population proportion. The assumptions were 95% confidence level or 5% margin of error and expected frequencies from studies done in Tigray Region and Kamba District. Thus, to calculate sample, three primary program performance indicators frequencies were taken from studies and largest of calculated sample was considered as representative [16,22]. The calculated and representative sample was 690 children represented by their OTP card (Table 1).
| Dependent variables | Confidence level (%) | Anticipated value (%) | Absolute precision | Design effect | Total sample size |
|---|---|---|---|---|---|
| Survival rate | 95 | 67.7 | 5 % | 2 | 690 |
| Default rate | 95 | 13.85 | 5 % | 2 | 364 |
| Death rate | 95 | 3.06 | 5% | 2 | 90 |
Table 1: Sample size determination for this study.
There are 12 Woredas in Wolaita administrative Zone. From this Woredas, four were selected by simple random sampling. The study area in average hold 4 health centers per Woreda and five satellite health posts per health center in their catchment area. Therefore, in average there are 20 health posts per Woreda in Wolaita Zone [23]. Of those health posts or OTP sites, 4 sites per each Woreda were selected through simple random sampling technique. Then, children at the site were admitted to sample by cluster sampling from respective sites (Figure 1).
Data collection procedures
Structured and pretested data collection checklists were used to collect data from both registration books and children OTP record. The records were reviewed mainly from children cards and some variables missing in cards were checked from registration book. Data collectors were 10+3 educational level in nursing and experienced with data collection. They were trained before data collection extensively.
Study variables
Dependent variable: Survival rate.
Independent variables: Age, sex, distance to OTP, type of malnutrition, physical examination and history at admission, length of stay, routine medications and seasonal variation.
Data quality control and management
Data were collected with close supervision at the time of collection. Subsequent to proper collection, data were carefully entered, thoroughly cleaned, coded and analyzed in SPSS version 20. Standard data cleaning procedures were carried out to assure data quality of both categorical and continuous variables [24].
Seasonal variations of admission and disparity in months were described across a year. Data were further analyzed by describing treatment outcomes by survival, death, and default rates [7]. Candidate variables for multivariate logistic regression were selected from bivariate logistic regression (P<0.25). Multivariate logistic regression was carried out to identify predictor variables of survival rate at 95% confidence level (AOR at 95% CI). Variables found associated with survival rate were tested for effect on survival status of children in the program through time by Kaplan-Meier survival curve and significance was reported by Log Rank test (P< 0.05).
Results
Socio-demographic characteristics of children at OTP, Wolaita Zone
From the total sample size calculated, 600(87%) were SAM based on management protocol and well registered. The rest 90(13%) were either none-SAM children or with large extent of missing information. Therefore, 600(87%) of participants were used for both descriptive and analytic processing. Of children included 353(53.8%) were female and 265(42.2%) were <24 months of age. Median age at admission was 24 months with IQR of (12 to 36). Children admitted from <25 km were 313(52.2%) with the mean distance of 25(14.1) km. Type of malnutrition were found as 395(65.8%) marasmic at their admission and children admitted with marasmic-kwash were 31(5.2%) of the participants (Table 2).
| Variables | Categories of variables | Frequencies | Percentage (%) |
|---|---|---|---|
| Age | < 24 months | 265 | 44.1 |
| > 24 months | 335 | 55.9 | |
| Sex | Female | 353 | 53.8 |
| Male | 247 | 46.2 | |
| Distance from OTP | < 24 km | 313 | 52.2 |
| > 25 km | 287 | 47.8 | |
| Type of malnutrition | Marasmus | 395 | 65.8 |
| Kwashiorkor | 174 | 29 | |
| Marasmic-kwash | 31 | 5.2 |
Table 2: Socio-demographic characteristics of SAM children admitted to OTP.
Seasonal variations of SAM admission to OTP at Wolaita Zone
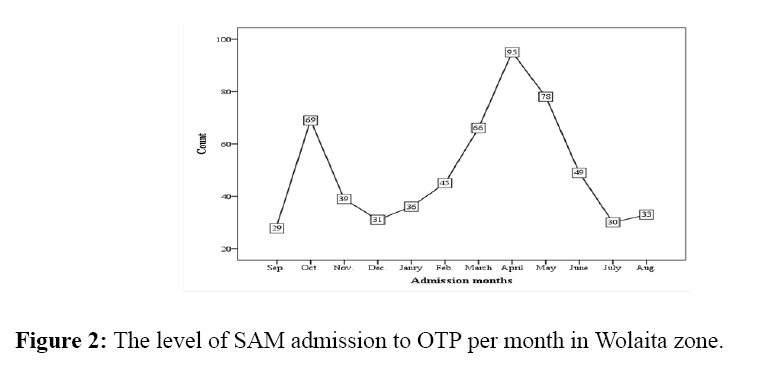
Children admitted to the program all over a year in the study area though varied among months. Large number of the participants were admitted in April 95(15.8%) and least admission of partakers admitted in September 29(4.8%) (Figure 2). Merging months to seasons, participants admitted from January to April (summer season) were 242 (40.3%). Least frequencies of the admissions were from September to December (winter season) 168 (28.0%) (Figure 3).
Treatment outcomes and Survival status of children admitted the program
Based on the finding of this study, survival rate was 396 (66.0%) of SAM children participated. Likewise, death and default rates were 4 (0.7%) and 10 (1.7%) respectively. Mean (SD) length of stay at OTP was 6.6 (2.24) weeks and children gain weight in average 2.2 g/kg/day for length of stay in the program (Table 3).
| Performance indicators | Frequencies indicators | International sphere standards references |
|
|---|---|---|---|
| Acceptable | Alarming | ||
| Survival rate | 396(66.0%) | >75% | <50% |
| Death rate | 4(0.7%) | <10% | >15% |
| Default rate | 10(2.3%) | <15% | >25% |
| Average weight gain | 2.2 g/kg/days | >8 g/kg/days | <8 g/kg/days |
| Length of stay | 6.60 weeks | <4 weeks | >6 weeks |
Table 3: Treatment outcomes of SAM children at OTP in Wolaita zone.
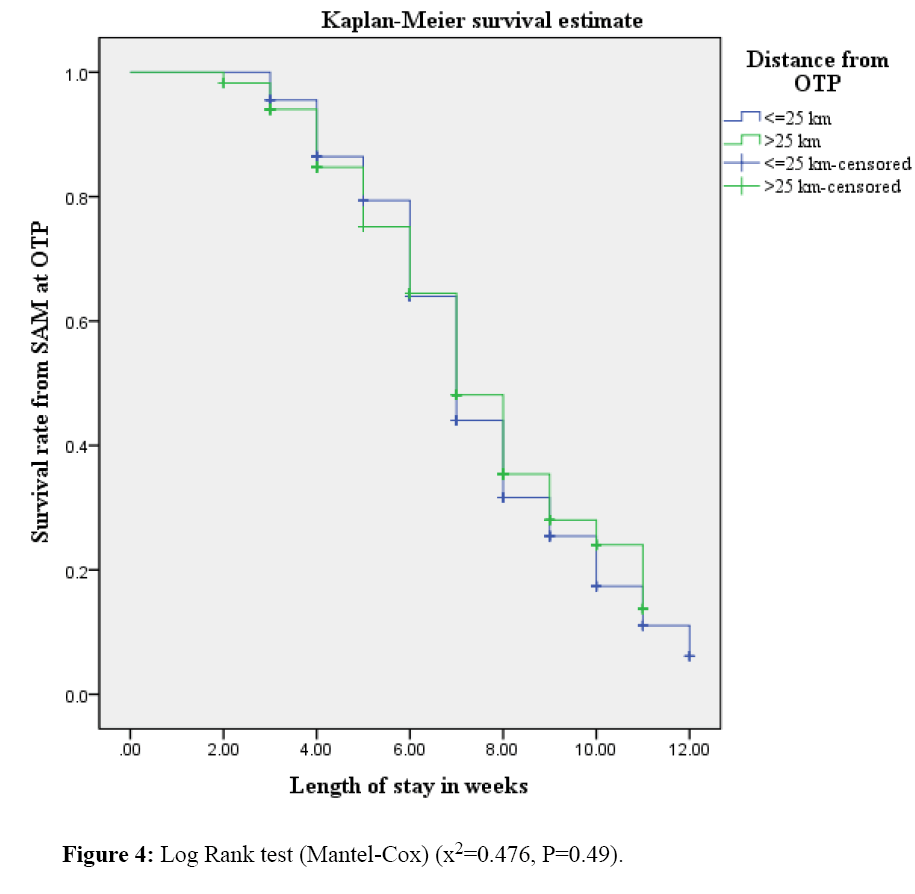
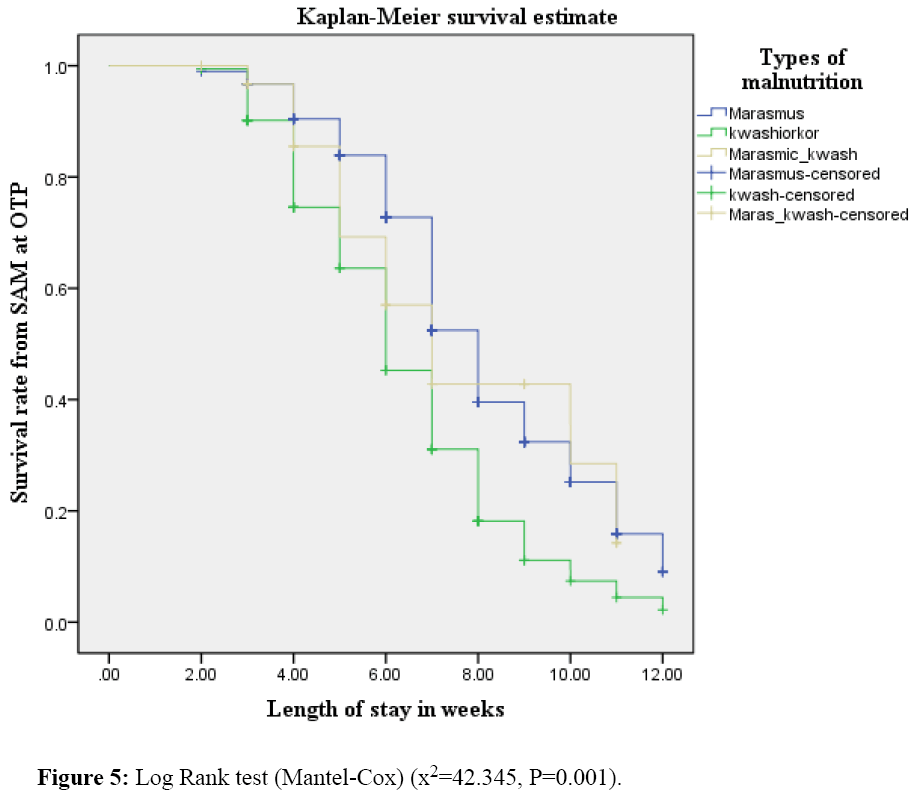
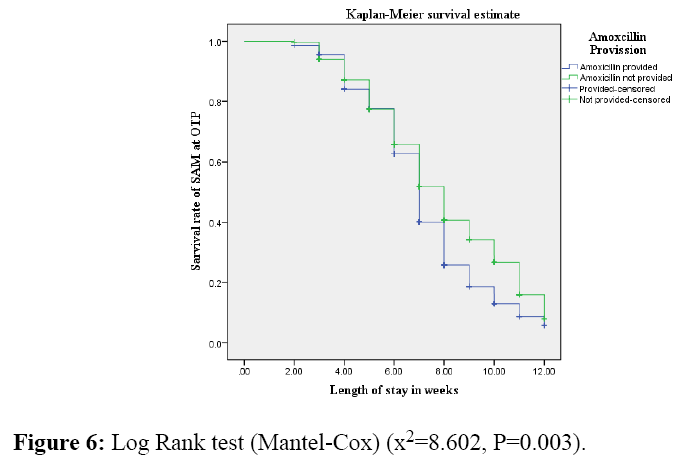
Children reside in <25 kms were with 1.74 times higher odds to survive than reside in >25 kms (AOR=1.74 at 95% CI (1.22, 2.48)) at multivariate regression. The likelihood of surviving was 2.96 times higher for children with kwash than marasmus (AOR=2.96 at 95% CI (1.99, 4.57)). Children provided amoxicillin were 1.66 times more likely to recover than their counterparts (AOR=1.66 at 95% CI (1.13, 2.37)). The effects of exposure variables on survival status of children through time were indicated by Kaplan- Meier survival curves underneath (Figures 4-6).
The probability of survival for children reside <25 km was 84% at fourth week of admission, but it was 80% for those in their counterparts in the same week. Yet, the discrepancy was not statistically significant by Log Rank test at 95% CI (P> 0.05). SAM children who were provided amoxicillin as supportive medication survived at fourth week for nearly 90% of participants and didn’t provide were survived almost 85% in the same week. Although, figures indicate as there is small difference among groups it was statistically significant at Log Rank test (P<0.05).
Discussions
The findings of this research mainly indicate seasonal distribution of SAM admission to OTP and children survival status through time per length of stay at Wolaita zone, Southern Ethiopia. The seasonal distribution of SAM admission indicates large numbers of children admitted to the program from January to April (summer season in Ethiopia) 242 (40.3%). The admissions from September to December (winter season) as 168 (28.0%) were seen as least figure. Children survival rate after full length of stay in the program was 396 (66.0%) and survival rate through time was affected in the significant level were: type of malnutrition and provision of supportive medication like amoxicillin at 95% confidence level in Log Rank test (P<0.05).
The survival rate reported as 396 (66.0%) at 95% CI of (62.2, 69.8) was lower than international sphere standard acceptable range [7]. The finding was also lower compared to 77.8% and 87% recovery rates from study done in TFC of Jimma and southern region [13,25]. Yet, it was in line to 58.1%, 61.8% and 67.7% rates from study done in OTP of sub-Saharan Africa, Tigray region and Kamba district respectively [4,16,22]. The discrepancies in the findings might be due difference in study settings (TFC and OTP).
The result indicates that the majority of cases 242(40.3%) with 95% CI of (36.2, 44.2) admitted to the program in summer season of the year in Ethiopia. This season is considered to be food scarce season. The reason is, up to January and/or later winter season is food harvest season in the study area; government and other food security supporting organizations didn’t recognize as food insecurity can happen like in the other seasons. Hence, most households exist without any support from organizations and other concerned bodies though Wolaita Zone is highly vulnerable area to food insecurity and malnutrition all over a year.26 Thus, larger admission rate of SAM children to OTP in this season might be due to lack of adequate outdoor body’s support in this season.
As stated survival status of children was significantly affected by type of malnutrition and provision of amoxicillin as supportive medication at Log Rank test (P<0.05). The finding was partially in agreement with study done in Tigray region as their report indicated recovery rate was significantly associated with amoxicillin provision as supportive medication [16]. Children admitted with kwashiorkor recover more likely than those with marasmus in study done at Kamba, which agrees finding of this study though focus is a bit side tracked in that study [22].
Limitation of the Study
The limitation of this study could be lack of household based variables which can have effect on survival status of children in the program. E.g. sharing of RUTF within families.
Conclusions
The findings of this study lead to conclude as large numbers of children were admitted to the program from January to April (summer season) in Wolaita Zone with the climax admission at April. That indicates as there is large seasonal variation in SAM admission rate to OTP in the study area. This program is evaluated by sphere standard acceptable ranges by their performance indicators. Thus, this study explored survival rate which is principal performance indicator and found as lesser than the sphere standard cut off points. In the other words, the program is not effective enough based on the sphere standard indicators. Variables which affect the survival status of children through time within length of stay were; type of malnutrition and provision of supportive medications like amoxicillin.
Recommendations
Considering the extent of admission rate variation by seasons, stakeholders should give attention in preparedness for vulnerable seasons.
Because supportive medications add significant input in the program effectiveness, consideration needed in provision of those medications like amoxicillin in the program
Moreover, because the program is in health post to have equipped experts, capacities building to service providers were recommended.
To reveal appropriate utilization of therapeutic foods at home and to identify program coverage further studies needed.
Ethical Considerations
Ethical clearance was obtained from the ethical review committee of the College of Health Sciences of Wolaita Sodo University. Letter of cooperation was obtained from Wolaita Zone health office for each selected Woreda and OTP sites. To obtain and differentiate specific child information, unique SAM number was used and observation was confidentially kept.
Competing Interest
The authors declare that they have no competing interests.
Acknowledgements
Authors would like to acknowledge data collectors and supervisors of this research for their sincere concern. Further, authors would like to extend deepest gratitude to NORHAD project for their financial support in the progress of the research work.
References
- UNICEF., WHO. WHO child growth standards and the identification of severe acute malnutrition in infants and children A Joint Statement by the World Health Organization and the United Nations Children’s Fund. WHO 2009.
- MOH. Jordan Guidelines for Management of Acute Malnutrition 2013.
- Hobbs B., Bush AA. Acute Malnutrition :An everyday emergency ; A 10-point plan for tackling acute malnutrition in under-fives, in Generation Nutrition campaign report 2014.
- Sadler K. Community-based Therapeutic Care: treating severe acute malnutrition in sub-Saharan Africa. Centre for International Health & Development Institute of Child Health UCL 2010.
- HTP, PART 2: Technical Notes, in Module 13,Management of severe acute malnutrition 2011.
- Müller O.,Krawinkel M. Malnutrition and health in developing countries. CMAJ 2005; 173: 279-286.
- Golden M., Grellety Y. Protocol for the management of Severe Acute Malnutrition, MOH, Editor. 2007, MOH: Ethiopia.
- Agency CS.EthiopiaDemographic and Health Survey, MOH, Editor. 2011: Addis Ababa, Ethiopia, Calverton, Maryland, USA.
- ENCU. Emergency Nutrition Quarterly Bulletin,Emergency Nutrition Coordination Unit Early Warning Department (Disaster Prevention and Preparedness Agency). 2008.
- UN. Nutrition Information in Crisis Situations Report n° 2 - Summary United Nations System Standing Committee on Nutrition May 2004.
- ENCU., EWRD. Emergency Nutrition Quarterly Bulletin,(Fourth Quarter 2008), in Emergency Nutrition Coordination Unit Early Warning & Response Department (Disaster Management & Food Security Sector). 2008.
- ENCU., DPPA. Emergency Nutrition,Quarterly Bulletin (Second Quarter 2008), in Emergency Nutrition Coordination Unit Early Warning Department (Disaster Prevention and Preparedness Agency). 2008.
- Teferi E., Lera M., Sita S., Bogale Z., Datiko DG., et al. Treatment outcome of children with severe acutemalnutrition admitted to therapeutic feeding centers in Southern Region of Ethiopia. Ethiop. J Health Dev 2010; 24: 3.
- UNICEF. Evaluation of Community Management of Acute Malnutrition (CMAM). Federal Ministry of Health, Government of Ethiopia and UNICEF Country Office, Ethiopia 2012.
- WHO.,UNICEF. Community-Based Management of Severe Acute Malnutrition A Joint Statement by the World Health Organization, the World Food Programme, the United Nations System Standing Committee on Nutrition and the United Nations Children’s Fund 2007.
- Yebyo HG., Kendall C., Nigusse D., Lemma W. Outpatient Therapeutic Feeding Program Outcomes and Determinants in Treatment of Severe Acute Malnutrition in Tigray, Northern Ethiopia: A Retrospective Cohort Study. PLOS ONE 2013; 8: 6.
- MOH, Integrated Management of Acute Malnutrition Guidelines M.O. Health, Editor. 2010: Republic of uganda.
- Charter H. Minimum standards in food security and nutrition. sphere hand book 2011.
- Burza S., Mahajan R., Marino E., Sunyoto T., Shandilya C., et al. Community-based management of severe acute malnutrition in India: new evidence from Bihar. Am J ClinNutr 2015; 101: 847-859.
- Misganaw C., Mesfin M.,Tesfaye M., DereseA. Retrospective study on outcome of in-patient treatment of Severe Acute Malnutrition in Jimma University specialized hospital from september 2011-september 2012. Journal of Diagnostics 2014; 1:18-28.
- Gebremichael M.,Bezabih AM.,Tsadik M. Treatment Outcomes and Associated RiskFactors of Severely Malnourished under FiveChildren Admitted to Therapeutic Feeding Centers of Mekelle City, Northern Ethiopia. Open Access Library Journal 2014; 1:1.
- Shanka NA., Lemma S.,Abyu DM. Recovery Rate and Determinants in Treatment of Children with Severe Acute Malnutrition using Outpatient Therapeutic Feeding Program in Kamba District, South West Ethiopia. Nutritional Disorders & Therapy 2015; 5: 2.
- WolaitaH. Zone Health Department, Annual report 2014.
- Unwin A. SPSS Survival Manual: A step by step guide to data analysis using SPSS for Windows (Version 12), J Pallant Editor 2005; Australia.
- Jarso HA., WorkichoA., Alemseged F. Survival status and predictors of mortality in severely malnourished children admitted to Jimma University Specialized Hospital from 2010 to 2012, Jimma, Ethiopia: a retrospective longitudinal study. BMC Pediatrics 2015; 15: 76.
- Jufare AT. Livelihood Adaptation, Risks and Vulnerability in Rural Wolaita, Ethiopia, in Environment and Development Studies. Norwegian University of Life Sciences: Norway 2008.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences