Political Economy of Poliomyelitis (India Case Study)
Samnani AA
Samnani AA*
Clinical Manager, Aahung NGO, Sexual and Reproductive Health Management Component,Karachi, Pakistan
- *Corresponding Author:
- Samnani AA
Clinical Manager
Aahung NGO
Sexual and Reproductive Health Management Component
Karachi, Pakistan
Tel: 923330377091
E-mail: am_samnani@hotmail.com
Abstract
Following successful elimination of smallpox globally, international health agencies united for eradication of polio. In 1988 World Health Assembly (WHA) passed a resolution to launch Global Polio Eradication Initiative (GPEI). India adapted GPEI in 1994 based on evidence of successful campaigns in regional countries. Program was piloted in 1994 and launched nationwide in 1995 as Pulse Polio Program (PPI) with the initial objective of eliminating polio by year 2000 and achieve polio free certification by year 2005. GPEI was spearheaded by World Health Organization (WHO), and worked in collaboration with different international agencies and was also supported by Government of India (GoI). From the very beginning PPI was publicized and supported by local health officials, politicians and celebrities. India was polio hyper-endemic country reporting almost 5000 polio cases annually in 1995. Until 1999 PPI relied on vaccinating children under 5, by conducting National Immunization Days (NIDs). National Polio Surveillance Program (NPSP) was established in 1997 for capacity building and reporting of disease. Over the years program faced many programmatic and implementation challenges leading to delay in achieving targets. Most important challenge was failure to vaccinate among few key challenges. To confront these challenges multiple innovative midcourse corrections were made including missed house strategy, transit point vaccination, new born tracking, vaccination of migratory population and vaccinating at special festivals like Eid, Diwali. Teams were trained to answer myths and beliefs of people regarding vaccine and approached religious leaders also for help. Research in field of vaccine was encouraged and more efficient monovalent OPV and later bivalent OPV were introduced to overcome vaccine failure. India reported last case of polio in 2011. Despite enormous and diverse population, unhygienic conditions and many other challenges India succeeded to eliminate polio by proper planning, sustained funding, clearly defined roles and responsibilities and timely monitoring and feedback.
Keywords
Abbreviations
AFP: Acute Flaccid Paralysis; CDC: Centers for Disease Control and Prevention; CGPP: CORE Group Polio Project; EPI: Extended Program Of Immunization; GEPI: Global Polio Eradication Initiative; GoI: Government of India; MoH: Ministry of Health; NID: National Immunization Day; NPSP: National Polio Surveillance Project; OPV: Oral Polio Vaccine; Polio: Poliomyelitis; PPI: Pulse Polio Immunization; RI: Rotary International; SMNets: Social Mobilization Network; SMO: Surveillance Medical Officer; SNID: Supportive National Immunization Day; UNICEF: United Nations Children’s Fund; USAID: U.S. Agency for International Development; WHA: World Health Assembly; WHO: World Health Organization; WPV: Wild Polio Virus
Background
The worldwide battle against polio began in 1988 with an introductory course of events to annihilate the infection by 2000. Notwithstanding actual progress in India just began in 1995 when worldwide organizations lined together with the Government of India (GoI) and local authoritative bodies, and large number of healthcare workers and social volunteers along with local resident gathered to dispatch a mass crusade. [1-3]
This policy analysis paper tries to articulate implementation issues related to polio eradication and lesson learned from India’s policy prescription using available policy tools and technology. The specialized impediments in India that were thought to be the most noticeably awful on the globe, hereafter unconquerable; in spite India's polio drive demonstrates that WPVs can be eradicated elsewhere where the hindrances are in fact less considerable. While India had the capacity to encounter the programmatic insufficiencies, somewhere else these stay imposing by virtue of socio-political reasons. [2,3]
Salient Features of the Policy
Following are the salient features of polio policy [3,4]
World Health Assembly (WHA) accentuated on need to actualize polio program in a manner to fortify routine health system functions.
Polio mass vaccination campaigns; with a specific end goal to enhance the scope routine inoculation by expanding immunization understanding.
Addressed social inequities in immunization coverage in regard to religion, gender, wealth, caste and race etc. and prevail over these disparities in immunization, for instance occupational caste identified by GoI as socially retrogressive are more inclined to be vaccinated as contrast with Scheduled position and the Scheduled tribes.
Maintain high level of vaccination coverage among children (at least 3 doses of OPV)
Developing sensitive system for lab and epidemiologic surveillance
Vaccinating all children during NIDs and SNIDs.
Mop up vaccination campaigns [3]
Rationale for Choosing the Particular Topic
Rationale for selecting India’s case study, lies in the story of eradicating polio and triumphant implementation of polices. India is the last one who thrives in eradicating polio. The Indian Polio eradication program studies have also underscore the post eradication polio strategy designed to capitalize on this new opportunity of polio free zone. Another reason being the similar nature of context and challenges as Pakistan is facing against polio.
Policy Analysis Framework used with Appropriate Justification
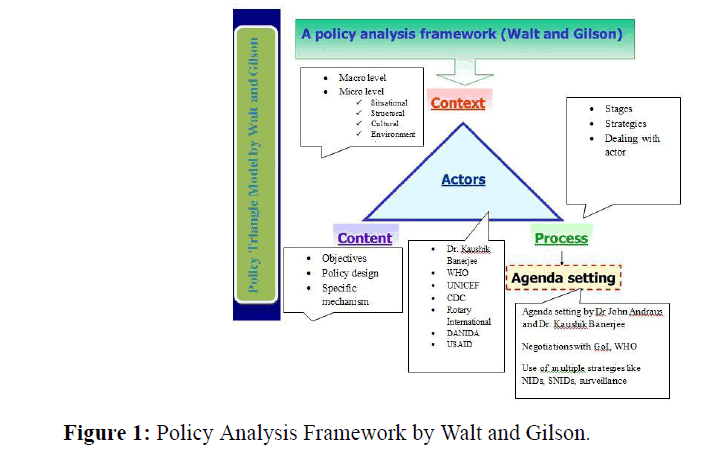
We are using Walt & Gilson triangle of policy analysis. The reason behind selecting Walt & Gilson model (1994) is its simple comprehensiveness that covers all the constituent of policy pillars and inter-linkage each entity (process, context, content and actors). Also it does not reject nor fully support either of the traditional approaches (rationalism and behaviorism). It juxtaposes both the approaches and incorporates their views by arguing the importance of policy content, context, process and role of actors (or Interest groups).
Since objectives of this paper is to look political economy of polio, so this model is the most appropriate one as it offers a broader framework and is closer to political economy approaches. Besides, this is a retrospective analysis and this triangle of policy analysis provides opportunity to analyze policy (Figure 1) prospectively as well as retrospectively. [5]
Context
Macro level factors
Global level: Polio eradication campaigns were very successful in America and Europe, followed by these encouraging results of polio campaign and successful elimination of Small pox.
Regional level: neighbouring countries like Thailand and Bangladesh conducted national immunization days in 1994-95 with successful coverage of 95% children under 5. Results were impressive and followed by a drop in new polio cases
National level: single disease (vertical) programs like malaria, TB control program were successful in India. [2] Successful elimination of small pox due to these single diseased and sharper focused programs laid strong foundation for polio eradication program. India adapted Extended Program of Immunization (EPI) in 1974, after its global launch by WHO in 1974.[6] OPV was included in EPI India in 1979 (in urban areas) and 1982 (rural areas).[7]
Situational: polio epidemic in late 80s on already hyper-endemic situation.
Structural: GoI mobilized all machinery to this cause, SMOs were deployed throughout country, volunteers, politicians, religious leaders stood for cause and volunteers and social mobilizers played important role.
Environmental: a global drive to polio, and donor assistance and funds flow for this cause.
Cultural: Myths regarding polio vaccination as an American maneuver to sterilize Muslim Population.
Content
Pulse polio immunization (PPI) program was launched in 1995 with objective of eradicating polio by the year 2000 and receiving eradication certificate by 2005. But later on these targets were revised as eradication of polio by year 2002, 2007.[8,9] Content is already mentioned under heading of Salient features.
Process
This was a top down approach, where international agencies took a lead role with support of GoI. Following this global drive for polio and donor support India piloted first polio campaign in New Delhi targeting one million children up to 3 years. One year later India launched nationwide PPI which focuses on vaccinating children under 5, by nationwide campaigns called as National Immunization Days (NIDs). During NIDs children were vaccinated at fixed booths twice a year. As a result WPV 2 circulation interrupted by 1999.[6] A strong surveillance program is needed for a successful disease control, so National Polio Surveillance Project (NPSP) is established for polio eradication in collaboration with DANIDA, WHO, CDC.[10]
PPI was very well publicized from very beginning as it gained support from local health officials, politicians and celebrities. [6,8]
In 1999 India was divided in low, medium and high risk areas, and SNIDs were held in medium and high risk areas.
UNICEF established Social Mobilization Network (SMNets) for social mobilization in 2001. Major task of these nets was to go into communities and counsel parents and educate them regarding any prevailing myths and misconceptions.[2]
Actors
Important stakeholders, their involvement and interest in issue and their power and positions are listed in following Table 1.
| Involvement in the issue | Interest in the issue | Influence/power | Position/ mobilization | ||||||
|---|---|---|---|---|---|---|---|---|---|
| International Actors | |||||||||
| World Health Organization (WHO) | High Policy formulation, Implementation |
High Training, immunization monitoring, , research, polio end game strategy, establishment of NPSP |
High Both at national and international levels |
Supportive | |||||
| Rotary International | High Policy formulation, Implementation Hygiene and health related activities |
High Creating awareness of campaign, Attracting donors, Advocacy and gaining confidence for campaign where there is resistance |
High | Supportive | |||||
| United Nations Children’s Fund (UNICEF) | High Procurement of vaccines until 2009, Social mobilization, research |
High | High | supportive | |||||
| CDC | High Formulation Implementation |
High | Medium | Supportive | |||||
| DANIDA | Moderate Implementation |
High Surveillance Establishment of NPSP |
Medium | Supportive | |||||
| Gates foundation | Moderate Implementation |
High Social mobilization Vaccine procurement |
Medium | Supportive | |||||
| Ministry of Health and Family Welfare, Government of India | High vaccine procurement, funding and logistics arrangement of campaign, mobilizing resources |
High Driving the program, coordinating with state governments |
High | Mixed (initially opposed, later supportive) | |||||
| National Polio Surveillance Project | High Hiring and training of vaccinators and SMOs |
High Surveillance of AFP |
High | Supportive | |||||
| India Expert Advisory Group | High Policy formulation Planning |
High | High | Supportive | |||||
| Political parties | Agenda setting Policy making Creating awareness |
Medium | High | Mostly supportive | |||||
| Celebrities | Marketing Creating awareness |
Medium | Medium | Supportive | |||||
| District Magistrate/ Zonal Head/Block Development Officer | High Implementation driving program at district level Mobilizing all departments |
High Executive head |
Medium to high | Supportive | |||||
| Local healthcare workers/ SMOs | High Micro planning , implementation of plans, communication with supervisors |
High maintaining quality of vaccines, ensuring delivery without any gap |
Low-medium | Supportive | |||||
| Village Panchayat/ women’s groups/social organizations | Implementation, Mobilizing communities |
Medium explaining importance of vaccination to community, creating awareness for campaign |
Low-medium | Supportive | |||||
| Dr John Andraus (adviser to WHO) | Negotiated with opposing groups, Coalitions with political parties. |
Advocated polio eradication on Epidemiological evidences | High | Supportive | |||||
| Dr.Kaushik Banerjee (Director EPI) | Negotiated with opposing groups, Coalitions with political parties. |
Advocated polio eradication on Epidemiological evidences | High | Supportive | |||||
Table 1: Role of actors, their involvement and interest in issue.
Process of Formulation and Implementation
Formulation
Agenda setting: Despite successful elimination of smallpox, many professionals and stakes holder were skeptical to adapt polio eradication, as they polio eradication beneficent to rich countries only. Polio advisor to WHO, Dr. Jon Andraus and Director of national immunization program of India. Dr. Kaushik Banerjee, were two persons who successfully negotiated with these opposing groups, and advocated polio eradication on strong epidemiological evidence of polio vaccine success in regional countries like Thailand and Bangladesh. Dr. Andrus made data rich presentation to MoH, showing success of polio vaccine globally. Besides MoH, Dr. Andrus and Banerjee made coalitions with political parties including BJP, which was in power in Delhi. In 1994 Health minister of Delhi, Harsh Vardhan announced 1st polio campaign on 2nd October (Mahatma Gandhi’s birthday). This was a big breakthrough and got support from all major political parties, as this campaign was launched on Mahatma Gandhi’s birthday.[3]
The difficulties the India has experienced amid plan setting were India's elected structure that entangles activity on a national scale (Unitary form of Government). The states have significant obligations regarding health not at all like USA which have federal form of government.
Implementation
This initiative was very flexibility in its implementation strategies. Micro plans were made at district level. A District task force (DTF) is formed which is controlled by the district magistrate. Different strategies involving traditional door to door campaigns and new innovative strategies like transit points and many more were introduces according to special needs and opportunities.
Serious issues encountered at implementation level such as: inaccessibility due to insecurity, sub-optimal performance of routine immunization, prevailing myths related to polio—infertility, the suspension of door-to-door activities in security-compromised high-risk districts/areas. All these issues were categorized as failure to vaccinate and failure of vaccine. To face these challenges multiple innovative midcourse corrections were made including missed house strategy, transit point vaccination, new born tracking, vaccination of migratory population and vaccinating at special festivals like Eid, Diwali. Teams were trained to answer myths and beliefs of people regarding IOPV. For this purpose support of local and religious leader were taken and also social mobilizing groups like SMNets were created. To face the challenge of failure of vaccine, research in field of vaccine was encouraged and more efficient mOPV and later bOPV were introduced.[3,4,6,11] India’s thickly densely populated cities; unhygienic conditions were also an important challenge encountered during implementation. UNICEF arranged health education sessions and water and sanitation (WASH) program to tackle this issue.
During the course of implementation the major challenges encountered by India; includes thickly populated states; both ecological and natural variables make for a high routine disease among Indian youngsters, the key populace for polio eradication (Table 2).
| Year | Number of polio cases reported | Activities |
|---|---|---|
| 1994 | 4791 | PPI piloted |
| 1995 | 3263 | PPI launched nationwide NIDs |
| 1997 | 2275 | NPSP established |
| 1999 | 2817 | Type 2 poliovirus eradicated. House-to-house strategy begins. IEAG for polio constituted |
| 2001 | 268 | Establishment of SMNet Amitabh Bachchan becomes UNICEF Brand Ambassador for Polio |
| 2002 | 1600 | GoI took lead in polio financing |
| 2003 | 225 | The under-served methodology was presented |
| 2004 | 134 | Transit immunization strategy suggested |
| 2005 | 66 | More effective monovalent OPV was introduced Intensification of Social mobilization, with high involvement of religious leaders |
| 2006 | 676 | Newborns tracking involving enumeration, vaccination started Revisit strategy to cover missed households missed house |
| 2007 | 874 | Formation of Ulemas' Committee to improve support of Muslim community |
| 2009 | 756 | Introducing geographically confound and very focused 107 Block plan |
| 2010 | 43 | Bivalent bOPV including type 1 and 3 WPV serotypes simultaneously was introduced Notification of GoI FOR Considering a single polio case as public health emergency |
Table 2: Chronology of events and number of cases reported in India.3,6
A strong monitoring and evaluation system was in place at all levels i.e. district, state and national to provide reliable and timely data for appropriate and immediate programmatic action.[4]
Reasons/ Factors for Success of Policy
Following are the key positive findings that turned into ultimate success [3]
Strong commitment of GoI
Joint efforts of international agencies and GoI
Clearly defined roles and responsibilities of people involved
Robust publicizing strategies
Adapting the basic concepts to local needs, in micro-communities and micro planning accordingly
Reconsiderations to the strategy looked in the form of multi-layered planning
Innovative techniques for marketing by involving celebrities
Community mobilization
Lessons and Policy Implications for Developing Countries
India’s polio eradication case is very important for three remaining polio endemic countries. Following policy implications can be drawn:
A disease eradication campaign is not just a medical affair as it is running in Pakistan (9) it involves inter-sectoral approach with interplay of government and non-government representatives including all relevant stakes holder like policy makers, policy implementers, clergy (regional ulema) and health workers.
To fill existing gaps by reinforcing routine and particular measures like NIDs and SNIDs
To avoid dependency on donors and foreign aid, encourage institutional capacity building and strengthening.
Proper implementation of polio eradication program is possible through considering content, contextual, operational, leadership, cultural and social factors along with surveillance and proper accountability.
Conclusion
Polio eradication is not medical affair only but it requires multidimensional understanding of social, cultural and health systems related realities and multi-sectoral approach is crucial for its eradication. Strong political commitment, sustained funding, multilayer planning, micro level implementation and timely feedback is key to success for achieving polio eradication.
Yet the biggest challenge is the post eradication phase. The key elements in global thinking is the about post eradication work are sustaining strong program of routine immunization, shifting from live to inactivated virus vaccine and maintain surveillance. The interplay of Macro and micro level factors are at high level and if contribution of these factors become strong and positive; these factors will ultimately transform challenges into triumphant.
References
- Aylward B., Tangermann R. The global polio eradication initiative: lessons learned and prospects for success. Vaccine 2011; 29: D80-D85.
- Coates EA., Waisbord S., AwaleJ., Solomon R., Dey R. Successful polio eradication in Uttar Pradesh, India: the pivotal contribution of the Social Mobilization Network, an NGO/UNICEF collaboration. Global Health: Science and Practice 2013; 1: 68-83.
- Schaffer TC. Polio eradication in India. Global Health Policy Center 2012.
- Thakur P. The Fight Against Polio: A Project Management Approach. 2014.
- Walt G.,Gilson L. Reforming the health sector in developing countries: the central role of policy analysis. Health policy and planning 1994; 9: 353-370.
- John TJ.,Vashishtha VM. Eradicating poliomyelitis: India's journey from hyper-endemic to polio-free status. The Indian journal of medical research2013; 137: 881.
- Lakhani D.,Bumb SS. Polio Eradication in India: A Journey from a Dream to Reality. International Journal of Scientific Study 2014; 1.
- BonuS., Rani M., Baker TD. The impact of the national polio immunization campaign on levels and equity in immunization coverage: evidence from rural North India. Social science & medicine2003; 57: 1807-1819.
- SathyamalaC., Mittal O., Dasgupta R., Priya R. Polio eradication initiative in India: deconstructing the GPEI. International Journal of Health Services2005; 35: 361-383.
- CDC., UNICEF., WHO. Journey to polio free India. 2012.
- HussainRS.,Mcgarvey ST., ShahabT., Fruzzetti LM. Fatigue and fear with shifting polio eradication strategies in India: a study of social resistance to vaccination. PloS one 2012; 7: e46274.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences