Left Pulmonary Vein Thrombus Extending into a Huge Left Atrium
Bolognesi M
Department of Internal General Medicine - AUSL della Romagna Cesena, Italy
- *Corresponding Author:
- Bolognesi M
Department of Internal General Medicine - AUSL della Romagna Cesena
Italy
Tel: +390547645074
E-mail: massimo.bolognesi@medici.progettosole.it
Clinical Presentation
Pulmonary vein thrombosis is an uncommon condition that is in most cases associated with major pulmonary surgery and lung malignancies. It has also been seen in cases of trauma, arteriovenous malformations, mitral stenosis, and atrial myxoma and, on occasion, no cause has been found [1]. Giant left atria are that chamber measuring larger than 8 cm and are typically found in patients who have rheumatic mitral valve disease with severe regurgitation and often atrial fibrillation. A huge left atrium may create the compression of the surrounding structures such as the esophagus, pulmonary veins, respiratory tract, lung, inferior vena cava, and lead to dysphagia, respiratory dysfunction, peripheral edema, hoarse voice, or back pain [2].
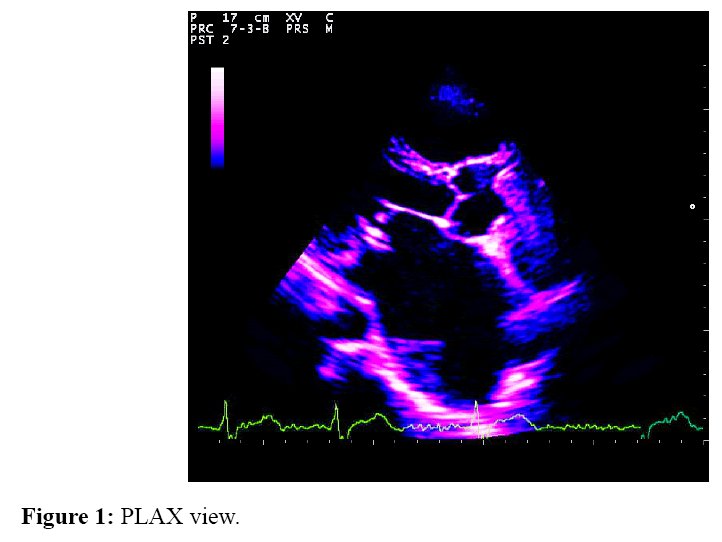
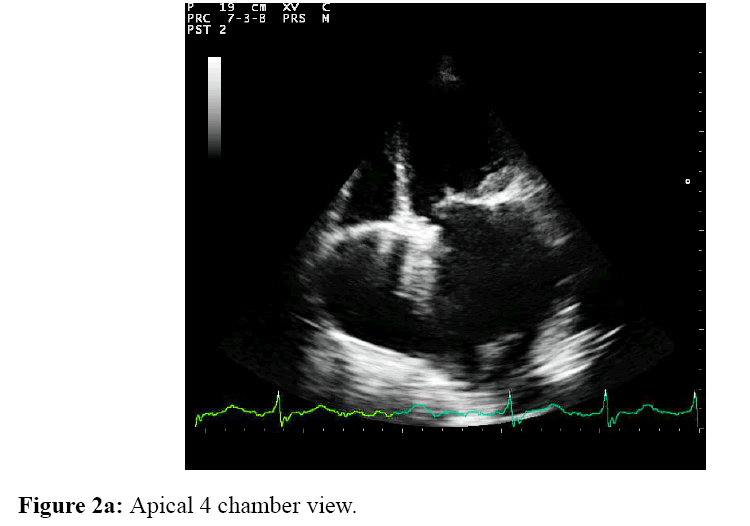
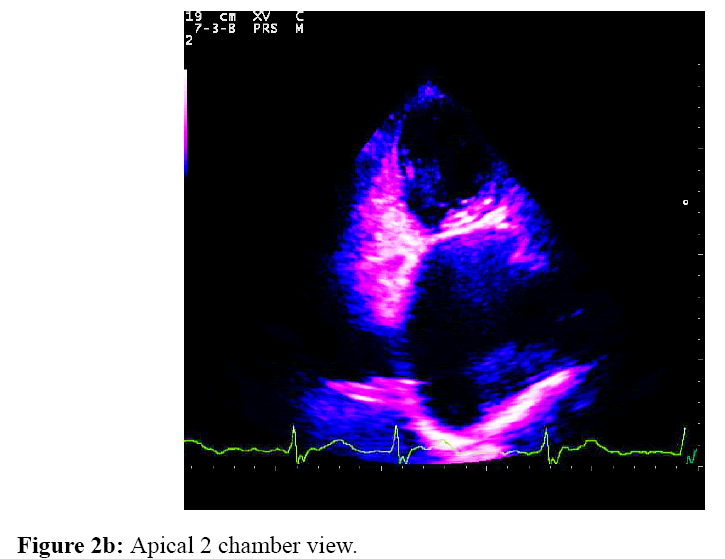
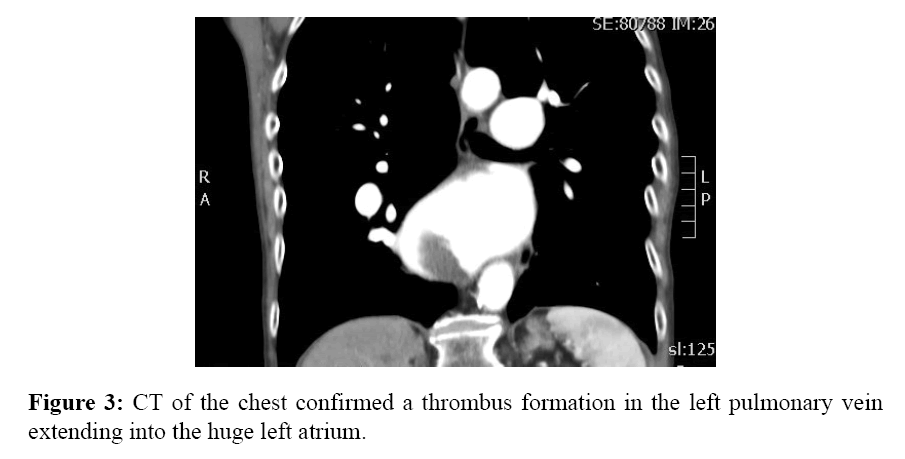
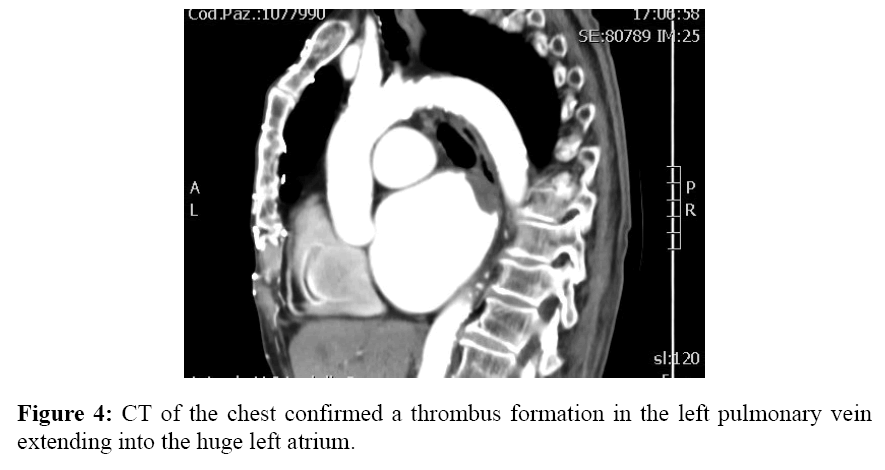
Herewith the author describes the interesting non-invasive cardiovascular findings with both Chest Computed Tomography and Two-Dimensional Transthoracic Echocardiography (2D TTE) performed in the setting of General Internal Medicine Department in a unhealthy 77-year-old female who suffered from long-standing rheumatic valvular heart disease and complained to paroxysmal nocturnal dyspnea with orthopnea. Firstly the 2D TTE showed a very enlarged left atrium with a thrombus which entering into the chamber from the left upper pulmonary vein (Figure 1-PLAX view, Figure 2a-Apical 4 chamber view, Figure 2b-Apical 2 chamber view). Subsequently, CT of the chest (Figures 3 and 4) confirmed a thrombus formation in the left pulmonary vein extending into the huge left atrium. The patient was successfully managed by double anticoagulation therapy with warfarin and low-density heparin.
References
- Cavaco RA., Kaul S., Chapman T. Idiopathic pulmonary fibrosis associated with pulmonary vein thrombosis: a case report. Cases Journal 2009; 2: 9156.
- Plaschkes J., Broman JB., Mercin G., Milwidsky H. Giant left atrium in rheumatic heart disease: a report of 18 cases treated by mitral valve replacement. Ann Surg1971; 174: 194–201.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences