Appropriate Radiologic Management of a Controversial Paraneoplastic Dermatologic Sign
Young CR, Wong EE
1Walter Reed National Military Medical Center, Bethesda, USA
- *Corresponding Author:
- Young CR
Walter Reed National Military Medical Center
Bethesda,USA
Tel: 3018758161
E-mail: colin.r.young.mil@mail.mil
Abstract
Leser-Trélat sign is a paraneoplastic disorder characterized by the eruptive appearance of multiple seborrheic keratoses. Leser-Trélat sign is generally associated with gastrointestinal adenocarcinoma; however, the association with malignancy is controversial. We present the case of a 37 year old male smoker, identified with Leser- Trélat sign and the ensuing clinical decision making and radiologic workup in search of underlying malignancy. Given the patient’s young age and smoking history, chest radiographs and age appropriate primary care managed cancer screening were chosen, in lieu of expensive, higher radiation dose, whole body imaging modalities such as PET or CT. The chest radiographs were normal, and the patient remains cancer free. Further research is needed to elucidate the underlying mechanisms of Leser-Trélat sign, validate its association with malignancy, and generate consensus evidence based medical guidelines with input from all specialties that manage oncologic patients to assist clinicians contain costs, minimize medical radiation exposure, and maintain high level diagnostic accuracy.
Keywords
Paraneoplastic, Sign of leser trélat, Radiologic management, Dermatologic management, PET-CT scan, Healthcare cost
Introduction
Several paraneoplastic disorders may be associated with the possibility of underlying malignancy. Some examples include musculoskeletal disorders (e.g. dermatomyositisis), reactive erythemas (e.g. erythema gyratum repens), vascular disorders (e.g. Trousseau's syndrome), papulosquamous dermatologic disorders (e.g. acrokeratosis paraneoplastica), and disorders of hair growth (e.g. hypertrichosis lanuginosa acquisita).[1,2] The clinical manifestations of these syndromes may precede, coincide with, or follow the diagnosis of cancer. Leser-Trélat sign is characterized as an eruptive appearance of multiple seborrheic keratoses historically associated with underlying malignant disease in medical literature. The abrupt appearance of copious seborrheic keratoses was first documented by two surgeons Edmund Leser and Ulisse Trélat,[3] and a later subsequent report clearly defined an association between this dermatologic event and cancer.[4] Leser-Trélat sign is usually associated with adenocarcinoma of the gastrointestinal tract, but may also occur in a vast array of others organs or herald other types of cancer including hematologic, soft tissue, and skeletal malignancies.[5-11] This paraneoplastic syndrome is thought to be related to a tumor-derived circulating growth factor, which induces epidermal proliferation and results in the rapid development of multiple seborrheic keratosis.[12]
However, seborrheic keratoses are extremely common with age and genetics being strong risk factors. Likewise, age and genetics are risk factors for many cancers. Various authors cast doubt on anything other than a mere coincidental association between cancer and Leser-Trélat sign.[13] These authors suggest that it would be useful to distinguish between a Leser-Trélat sign and a Leser-Trélat syndrome. They propose that Leser-Trélat sign be defined as a sudden acute emergence of seborrheic keratoses sometimes accompanied by pruritus or acanthosis nigricans. According to this definition, Leser- Trélat sign may be present with or without occult malignancy and is detectable with history and physical examination alone. The Leser-Trélat syndrome would describe a paraneoplastic syndrome in patients with the Leser-Trélat sign in whom an occult malignancy was identified after the appearance of the sign. Supporting these authors proposal, Leser-Trélat sign has been described in many nonmalignant conditions including HIV infection,[14] generalized dermatitis,[15] and heart transplant.[16] Other case reports describe the appearance of the Leser-Trélat sign and completion of expensive diagnostic workups followed by multiple years of surveillance without the appearance of malignancy.[17]
We present a case of a young patient identified with the controversial Leser-Trélat sign and the ensuing clinical decision making and radiologic workup in search of underlying malignancy.
Case Report
An overweight 37 year old male US Army Reservist was seen in Dermatology clinic due to a suspected dermatofibroma on his left elbow. The lesion was excised and pathology confirmed the suspected diagnosis. Incidental to this visit, the physician observed and the patient endorsed a recent eruption of multiple seborrheic keratosis following a distal clavicle resection due to impingement ten days earlier. His past medical history was significant for moderately controlled hypertension on Lisinopril 20 mg daily, and hyperlipidemia. The patient endorsed a half pack per day cigarette smoking habit, in excess of twenty years.
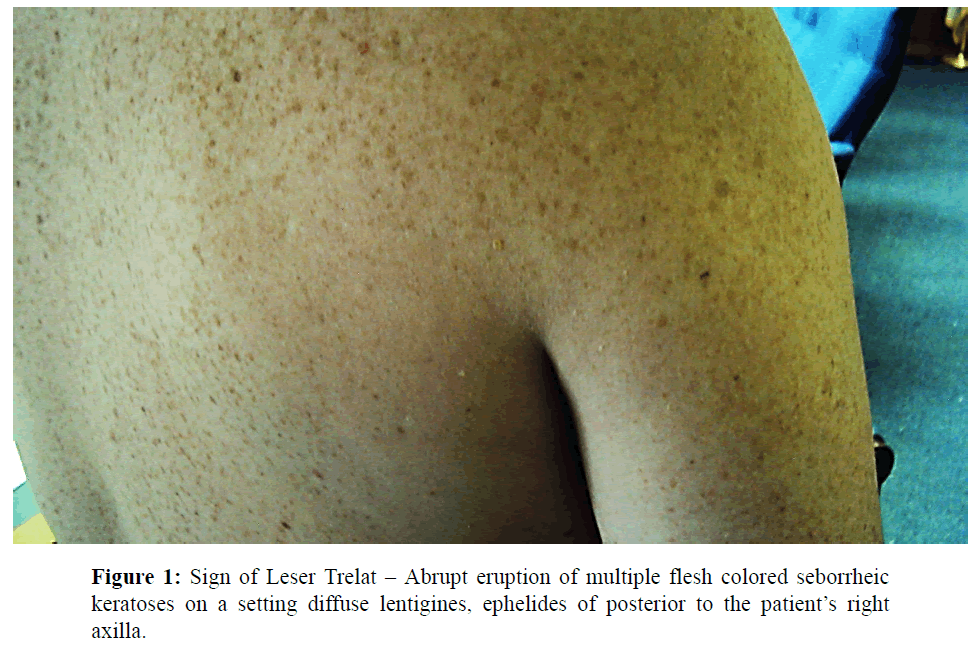
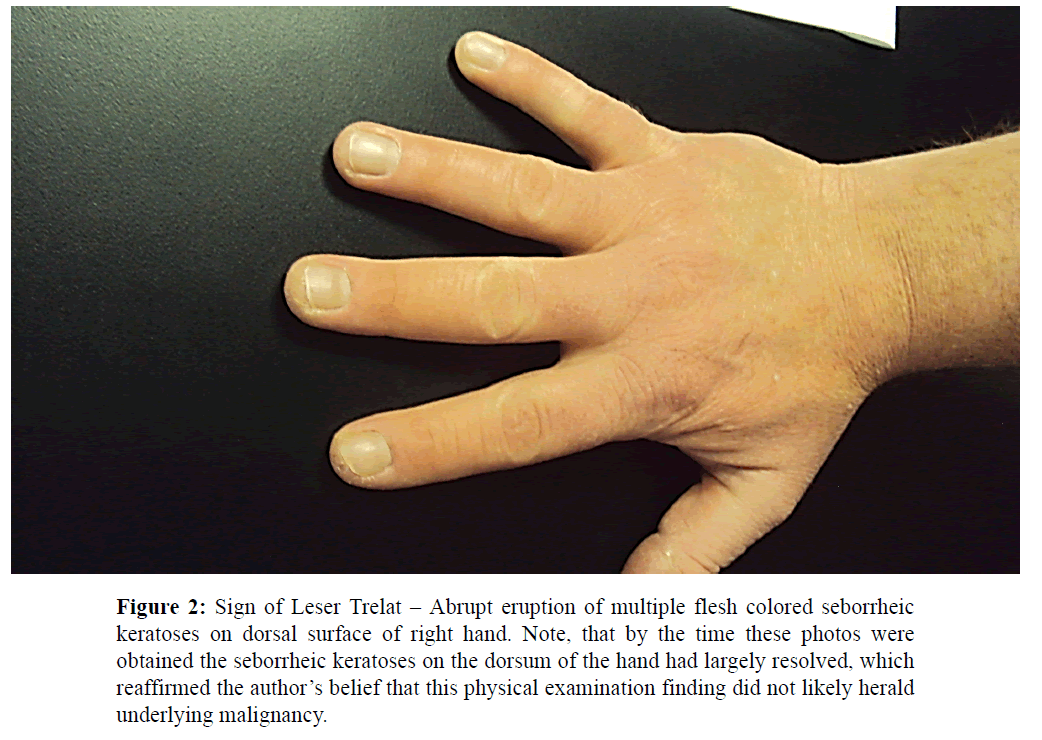
Dermatologic examination revealed a male with type 1 skin with scattered flesh colored, stuck-on appearing papules and plaques, too numerous to count, on the posterior to his axilla bilaterally and to a lesser extent on the dorsum of his hands consistent with stucco and seborrheic keratoses (Figures 1 and 2).
Figure 2: Sign of Leser Trelat – Abrupt eruption of multiple flesh colored seborrheic keratoses on dorsal surface of right hand. Note, that by the time these photos were obtained the seborrheic keratoses on the dorsum of the hand had largely resolved, which reaffirmed the author’s belief that this physical examination finding did not likely herald underlying malignancy.
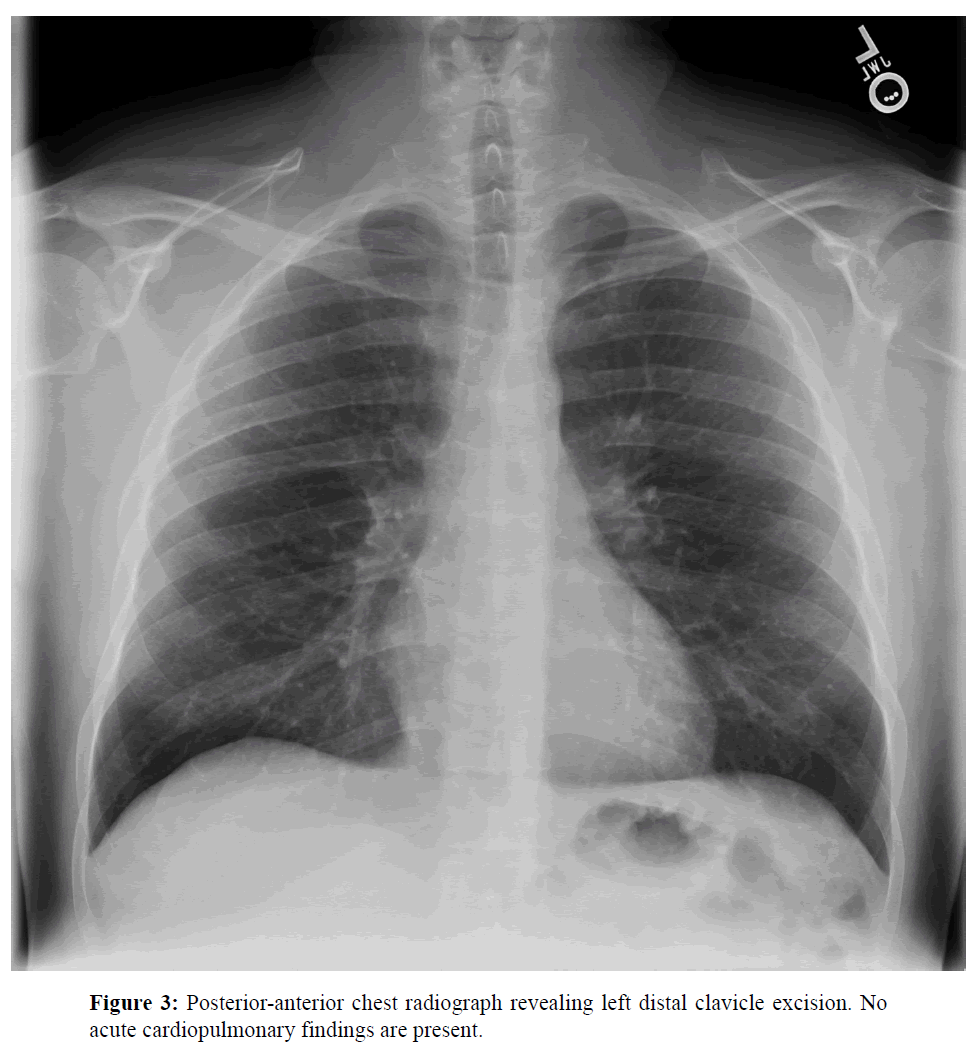
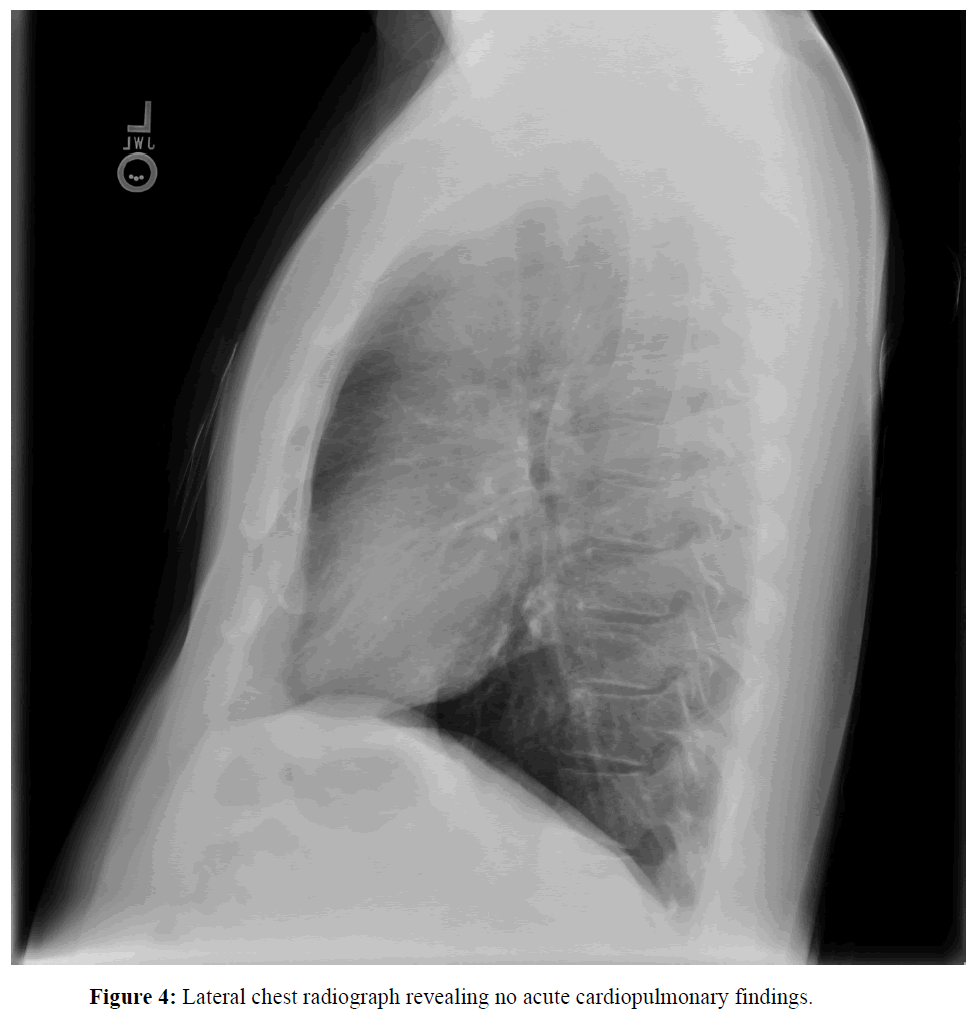
Given the patient’s considerable tobacco history and the identification of Leser-Trélat sign, plain film chest radiographs were ordered by dermatology to evaluate for pulmonary malignancy and the patient was referred back to primary care for further age appropriate cancer screening. The posterior to anterior and lateral radiographs revealed no acute cardiopulmonary disease (Figures 3 and 4). The attending radiologist suggested considering a positron emission tomography coupled with computed tomography (PETCT) scan if clinical suspicion of occult malignancy was high.
The patient declined histopathologic sampling of the lesions. The majority of the lesions on the dorsum of the patient’s hands, which had been classified clinically as seborrheic keratoses by the dermatologist, resolved within one month of onset.
Discussion
Above, we present a case of a patient identified with the Leser-Trélat sign and the ensuing clinical decision making and radiologic workup in search of underlying malignancy. Leser-Trélat is a controversial paraneoplastic dermatologic sign of internal malignancy. In our case report, the attending physician (i.e the dermatologist) elected to use plain film chest radiographs to evaluate for lung cancer given the patient’s significant tobacco history, in addition to standard primary care managed age appropriate cancer screening (e.g. colonoscopy). Given, that the average age of appearance of Leser-Trélat sign is approximately sixty years old when associated with underlying malignancy,[17] this management choice seems reasonable, despite the reports of malignancy accompanying Leser-Trélat sign in young adults.[9] An alternative explanation, for the appearance of the Leser-Trélat sign in this patient may be that immune and inflammatory cytokines were released in response to the surgical stress or opioid pain control from the patient’s recent distal clavicle resection subsequently initiating a dermatologic reaction. This is consistent with other case reports in which Leser-Trélat sign appeared shortly after surgery.[16]
An alternative management choice would have been an expensive whole body PET-CT scan [approximately 1500-3000 US dollars18], or chest/abdomen/pelvis CT scan [approximately 650-1200 US dollars19,20], in an aggressive, non-invasive whole body search for malignancy, instead of a chest radiograph [approximately 70 US dollars21]. PET-CT has poor sensitivity for some gastrointestinal malignancies22 and thus may not be an ideal screening tool. In this case, the selection of chest radiographs with a total effective dose equivalent (TEDE) between 0.06 and 0.25 milliseverts [23] spared the patient a TEDE of approximately 25 milliseverts [24] from a whole body PET-CT scan, a radiation dose reduction of at least two orders of magnitude. One could argue that no further work up is warranted other than periodic surveillance due to the questionable positive predictive value of Leser-Trélat sign for malignancy especially amongst young patients. Generation of consensus evidence based medical guidelines with input from all specialties that manage oncologic patients is needed to assist clinicians contain costs, minimize medical radiation exposure, and maintain diagnostic accuracy when managing controversial paraneoplastic signs including Leser-Trélat. The patient was counseled on the potential risks and benefits of the both clinical decision alternatives and expressed desire to not undergo PET-CT imaging for Leser-Trelat sign.
In summary, the association between Leser-Trélat sign with underlying internal malignancy is controversial, and appropriate clinical management is subject to interpretation and is case dependent. The authors propose that the work up for patients with the Leser-Trélat sign include a full history and physical by their primary care provider and testing directed by pertinent positives on history, review of systems, physical examination or based on risk factors (e.g. smoking, intravenous drug use, asbestos exposure). All patients with a potential paraneoplastic syndrome should use the opportunity to get their age-appropriate cancer screening updated (e.g. well woman exam, colonoscopy, mammography). More expensive testing such as PET-CT scan maybe warranted if clinical suspicion for occult malignancy remains high. Further research is needed to elucidate the underlying mechanisms of Leser-Trélat sign, and generate consensus evidence based medical guidelines with input from all specialties that manage oncologic patients to assist clinicians contain costs, minimize medical radiation exposure, and maintain a high level of diagnostic accuracy.
Disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, nor the United States Government.
Acknowledgment
The authors are military service members. This work was prepared as part of the authors official duties. Title 17 U.S.C 105 provides that ‘Copyright protection under this title is not available for any work of the United States Government.’ Title 17 U.S.C. 101 defines a U.S. Government work as a work prepared by a member or employee of the U.S. Government as a part of that person’s official duties.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
References
- Lee A. Skin manifestations of systemic disease. AustFam Physician 2009; 38: 498-505.
- Ponti G., Luppi G., Losi L., Giannetti A., Seidenari S. Leser-Trélat syndrome in patients affected by six multiple metachronous primitive cancers. J HematolOncol 2010; 3: 2.
- Leser E. Ueberein die Krebskrankheitbeim Menschen haufigbegleitendes, nochweniggekanntes Symptom. Munchener Med Wochenschr 1901; 51:2035-2036.
- Hollander EV. BeitragezurFruhdiagnose des Darmcarcinomas (Hereditatsverhaltnisse und Hautveranderungen). Deutsche MedicinischeWochenschrift 1900; 26: 483-485.
- Lilly E., Granter SR., Haynes HA., Ibrahimi OA. Chemotherapy-induced inflammatory seborrheickeratoses in a man with acute myeloid leukemia: a variant of Leser-Trélat sign?. Cutis 2012; 90: 235-236.
- Lindelöf B., Sigurgeirsson B., Melander S.Seborrheickeratoses and cancer. J Am AcadDermatol1992; 26: 947-950.
- Schwengle LE., Rampen FH., Wobbes T.SeborrhoeicKeratoses and internal malignancies. A case control study. ClinExpDermatol 1988; 13: 177-179.
- Siedek V., Schuh T., Wollenberg A.Leser–Trelat sign in metastasized malignant melanoma.Eur Arch Otorhinolaryngol 2009; 266: 297–299.
- Barron LA., Prendiville JS. The sign of Leser-Trélat in a young woman with osteogenic sarcoma. J Am AcadDermatol1992; 26: 344-347.
- Yavasoglu I., Kadikoylu G., Bolaman Z. The Leser-Trelat sign is an associated with acute myeloid leukemia.Ann Hematol 2011; 90: 363.
- Al Ghazal P., Körber A., Klode J., Dissemond J.Leser-Trélat sign and breast cancer. Lancet 2013; 381: 1653.
- Ellis DL., Kafka SP., Chow JC., Nanney LB., Inman WH., et al. Melanoma, growth factors, acanthosisnigricans, the sign of Leser-Trélat, and multiple acrochordons. A possible role for alpha-transforming growth factor in cutaneous paraneoplastic syndromes. N Engl J Med 1987; 317: 1582-1587.
- Heaphy MR Jr., Millns JL., Schroeter AL. The sign of Leser-Trélat in a case of adenocarcinoma of the lung.J Am AcadDermatol2000; 43: 386-390.
- Inamadar AC., Palit A. Eruptive seborrhoeic keratosis in human immunodeficiency virus infection: a coincidence or 'the sign of Leser-Trélat'?.Br J Dermatol. 2003; 149: 435-436.
- Schwengle LE., Rampen FH. Eruptive seborrheickeratoses associated with erythrodermicpityriasisrubrapilaris. Possible role of retinoid therapy. ActaDermVenereol 1988; 68: 443-445.
- Hsu C., Abraham S., Campanelli A., Saurat JH., Piguet V. Sign of Leser-Trélat in a heart transplant recipient. Br J Dermatol.2005; 153: 861-862.
- Safa G., Darrieux L.Leser-Trélat Sign without internal malignancy.Case Rep Oncol 2011; 4:175-177.
- Verboom P., van Tinteren H., Hoekstra OS., Smit EF., van den Bergh JH., et al. Cost-effectiveness of FDG-PET in staging non-small cell lung cancer: the PLUS study. Eur J Nucl Med Mol Imaging2003; 30: 1444-1449.
- Hunink MG., Bos JJ. Triage of patients to angiography for detection of aortic rupture after blunt chest trauma: cost-effectiveness analysis of using CT. Am J Roentgenol 1995; 165: 27-36.
- Mindelzun RE., Jeffrey RB. Unenhanced helical CT for evaluating acute abdominal pain: a little more cost, a lot more information. Radiology1997; 205: 43-45.
- Wiencek RG., Weaver DW., Bouwman DL., Sachs RJ. Usefulness of selective preoperative chest x-ray films. A prospective study. Am Surg1987; 53:396-398.
- Skehan SJ., Brown AL., Thompson M., Young JE., Coates G., et al. Imaging features of primary and recurrent esophageal cancer at FDG PET. Radiographics 2000; 20: 713-723.
- Simpson AK., Whang PG., Jonisch A., Haims A., Grauer JN. The radiation exposure associated with cervical and lumbar spine radiographs. J Spinal Disord Tech 2008; 21:409-412.
- Brix G., Lechel U., Glatting G., Ziegler SI., Münzing W., et al. Radiation exposure of patients undergoing whole-body dual-modality 18F-FDG PET/CT examinations. J Nucl Med 2005; 46:608-613.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences